Explore 2020 Research
The efficacy of high versus low dose exercise for rotator cuff disease
| Funded by: | Arthritis South Australia and Arthritis Australia |
| Recipient: | A/Prof Peter Malliaras |
| Intended Department | Physiotherapy, Monash University |
| Project: | The efficacy of high versus low dose exercise for rotator cuff disease |
Scientific summary:
What were the main scientific objectives of the grant?
The primary scientific objectives of the grant were to assess the feasibility of a fully powered, multicentre randomized controlled trial comparing the efficacy of high load-volume versus low load-volume exercise interventions for rotator cuff tendinopathy.
Specifically, the study aimed to evaluate the recruitment rate, retention rate, adherence to the prescribed exercise regimen, and completion rate of follow-up questionnaires. Additionally, the study sought to compare the clinical outcomes between the two exercise interventions, focusing on shoulder pain and disability index (SPADI), pain intensity (visual analogue scale), and one repetition maximum (1RM) strength measurements.
The research aimed to identify the most effective exercise variables for treating rotator cuff tendinopathy and to ensure the safety and tolerability of the interventions.
What were the main scientific achievements of the grant?
The trial provided valuable data on the adherence rates and retention of participants over a 26-week period. The retention rates were 83.9% at 6 weeks and 80.6% at both 12 and 26 weeks, indicating strong participant engagement throughout the study. Additionally, the completion rates for follow-up questionnaires were relatively high, although slightly below the predefined success criteria.
Clinically, both high load-volume and low load-volume exercise interventions led to improvements in shoulder pain and function, as measured by SPADI and visual analogue scale scores. Notably, the high load-volume group exhibited greater gains in 1RM strength tests, suggesting that higher intensity exercises may be more effective for enhancing strength in individuals with rotator cuff tendinopathy.
However, the study also identified challenges, such as slightly lower adherence rates to the prescribed exercise regimens and increased reports of shoulder pain requiring additional analgesia in the high load-volume group. These findings suggest the need for improved methods to monitor and support exercise adherence.
Overall, these outcomes lay the groundwork for future research aimed at optimizing rehabilitation strategies for rotator cuff tendinopathy.
What problems, if any, did you encounter in achieving the project’s objectives, and how did you address them?
There were no issues outside of the usual challenges encountered in running a randomised trial
What is the plan for dissemination of findings?
The findings have been included within a PhD thesis and are now under review for publication in a peer reviewed scientific journal.
Lay summary:
Overview:
This study looked at how different exercise programs can help people with rotator cuff tendinopathy, a common shoulder problem causing pain and difficulty in moving. We wanted to find out if doing exercises with weights is better than doing the same exercises without weights.
We asked 31 people with shoulder pain to join our study. They were split into two groups: one group did exercises using dumbbells, and the other group did the exercises without any added weight. They followed these exercise plans for 12 weeks, with up to seven sessions guided by a physiotherapist.
We wanted to see if we could successfully run a larger study comparing these two types of exercise programs. We aimed to learn how well people would stick to the exercise plan and how it would affect their shoulder pain and strength.
Most people completed their exercises and filled out the follow-up questionnaires. Both groups saw improvements in their shoulder pain and function, but those who used weights got stronger. Overall, our study shows it’s possible to run a bigger trial to compare these exercise programs. Future studies should find ways to help people stick to their exercises and manage any pain they might feel. This research helps us understand how different exercise types can improve shoulder pain and strength.
What problems did you try to solve, or gaps in knowledge did you try to fill?
The study aimed to answer whether high load-volume exercises (using weights) are more effective than low load-volume exercises (no weights) for treating rotator cuff tendinopathy. We sought to solve the problem of unclear exercise guidelines by comparing the two exercise intensities. This is important because rotator cuff tendinopathy affects many people, causing long-term pain and disability, and exercise is a key treatment. By identifying the most effective exercise approach, we can improve rehabilitation strategies, reduce pain and disability, and enhance the quality of life for those affected by this common shoulder condition.
What did you discover during the course of the grant?
During the study, we discovered that using social media for recruitment was highly effective, allowing us to enroll 31 participants in just two months. This success suggests that similar methods could be used for larger studies. Both high load-volume (using weights) and low load-volume (no weights) exercise programs improved shoulder pain and function. However, the group using weights saw greater strength gains, indicating that higher intensity exercise may be more beneficial for building strength.
We also found that adherence to the exercise programs was slightly below our target, particularly in the high load-volume group. Some participants in this group experienced increased shoulder pain, requiring extra pain relief.
Participant retention and questionnaire completion rates were high, showing strong engagement throughout the study. These findings suggest that a larger trial is feasible and can provide valuable insights into the best exercise practices for treating rotator cuff tendinopathy. Overall, our pilot trial demonstrated the potential benefits of different exercise intensities and provided important information for future research and clinical applications.
Have the findings of the research already benefited people with musculoskeletal disease? How might the findings inform further research to help sufferers in the future?
The findings have not yet directly benefited people with musculoskeletal disease but provide a foundation for future studies. This research informs further trials by highlighting the importance of exercise intensity and adherence. Future research can build on these insights to develop more effective, personalized rehabilitation programs, ultimately improving outcomes for those with rotator cuff tendinopathy.
Are you planning to continue the research?
We are cautious about moving to a full-scale trial due to the limited differences in pain benefits between the groups. The next steps involve rethinking the study design to address adherence issues. Our team is currently working in technology that can measure how much exercise people do more accurately which could be used in a future trial to more accurately assess the relationship between exercise and patient benefit.
Knee Osteoarthritis - A focus on walking
| Funded by: | Heald Fellowship ARA 2020 |
| Recipient: | Dr Saliu Balogun |
| Intended Department | Menzies Institute for Medical Research – University of Tasmania |
| Project: | A randomised controlled trial evaluating community walking for knee osteoarthritis |
Exercise can reduce symptoms in patients with knee osteoarthritis and may also benefit from reducing the elevated risk of cardiovascular diseases such as ischemic heart disease and congestive heart failure in these individuals. Yet, the uptake of exercise by patients with knee osteoarthritis is poor. One of the most common myths is that exercise will cause damage to an already worn joint (particularly weight-bearing exercise). To dispel the fears that weight-bearing exercise, such as walking, is detrimental to knee structure, new knowledge is required to show its safe and does no harm to the knee joint. Such knowledge would have major implications, as it would dispel the fears around weight-bearing exercise, providing clinicians with the evidence base to confidently prescribe walking and reassuring patients to follow this advice. Greater uptake of exercise in this patient group is likely to result in greater symptomatic benefits, leading to a reduced/prolonged need for knee replacement surgery. Furthermore, dispelling the fear that exercise is damaging to the knee structures is likely to encourage physical activity participation in individuals with knee osteoarthritis, thus reducing the elevated risk of cardiovascular diseases including ischemic heart disease and congestive heart failure among these individuals. To date, there have been limited studies examining the effect of exercise on MRI-assessed knee joint structure. My project is a pilot randomised controlled trial (RCT) aimed to test the feasibility of an aerobic outdoor community walking intervention. The secondary objective was to provide exploratory information on the magnitude and direction of effect sizes for pain, function, stiffness, and MRI knee structural change.
This study demonstrated the feasibility of enrolment, adherence, and safety of implementing an aerobic outdoor community walking intervention among patients with knee osteoarthritis.
Feasibility of enrolment: Over nine months, 49 individuals were screened for eligibility, with 40 enrolled (24 randomised to walking and 16 randomised to usual care). We could not achieve our target sample size of 48 due to budgetary constraints. Randomisation worked relatively well given the small study sample: The baseline characteristics of the two groups were generally well balanced, apart from the walking group having slightly more females (62.5% vs 56.3%), having a higher BMI (33.6 vs 31.8), and having a lower proportion of varus aligned knees compared to the usual care group (66.7% vs 87.5%).
Adherence: Over 24 weeks mean adherence was 70.0% (85.1% for the first 12 weeks and 54.9% for the second 12 weeks). All participants who withdrew (n=7) were from the walking group.
Safety of intervention: Walking was safe, and the adverse events related to the intervention were low. There were more adverse events in the walking group (26 vs 8), of which the majority were mild and classified as musculoskeletal. Some of the adverse events reported include increased knee pain, foot pain, upper body pain, plantar fasciitis, and calf strain.
Although a pilot study, this trial showed that a community walking intervention led to clinically and statistically significant improvements in pain, function and stiffness, and performance of the 30s Chair Stand Test. The changes seen in MRI joint structure over 24 weeks can be used to inform the development of a larger, more definitive study to determine structural changes related to walking.
The study’s abstract has been accepted for a poster/rapid-fire presentation at the 2021 OARSI Virtual World Congress on Osteoarthritis. In addition, the project also attracted an Honours student who has now submitted his honour’s thesis.
Development fo a novel SLE therapeutic
| Funded by: | Heald Fellowship ARA 2020 |
| Recipient: | Dr Jacqueline Flynn |
| Intended Department | School of Clinical Sciences- Monash University |
| Project: | Development fo a novel SLE therapeutic |
Glucocorticoids have been used for over 60 years as the mainstay treatment for autoimmune diseases. Despite their widespread use, glucocorticoids cause debilitating side effects including osteoporosis, diabetes, organ damage and heart disease. Systemic lupus erythematous (SLE) is an incurable autoimmune disease where disease severity is mediated by type I interferons (IFNs).
Important for SLE patients, our study investigated a novel regulator of type I IFNs called GILZ. We and others have previously illustrated that GILZ displays many of beneficial anti-inflammatory effects of glucocorticoids, but without the detrimental metabolic side effects. Additional to these benefits, this study importantly demonstrated that GILZ negatively correlated with disease activity in SLE patients. Significantly we also demonstrated that GILZ is able to regulate type I IFNs, which is key as type I IFNs correlate with SLE disease severity. Thus, this body of research indicates that GILZ represents a unique checkpoint on the IFN program. Although further research is required, the findings of this study highlight the importance of examining GILZ, as a potential therapeutic target, in future SLE therapies.
You can read more about this project here: Scientific Summary – Dr Jacqueline Flynn
The Interlock Study
| Funded by: | Arthritis Australia |
| Recipient: | Ms Hema Urban |
| Intended Department | Kolling institute of Medical Research / University of Sydney |
| Project: | The Interlock Study |
The Arthritis Australia scholarship has supported me for a very productive 1-year FTE equivalent administered from January 2019 to March 2020 in the Doctor of Philosophy degree at The University of Sydney. The project submitted for this application was entitled the INTERLOCK study which intended to evaluated laboratory and clinical outcomes of the infrapatellar fat pad (IFP) in end-stage knee osteoarthritis (OA) patients undergoing total knee replacement. Administrative paperwork and protocol establishment for flow cytometry was carried out before recruitment commencing in February 2019. However, due to insufficient subjects, the recruitment strategy was revised in May 2019 with an additional three months to assess the effectiveness of changes. In total, 4 participants were recruited over six months and hence the study was deemed not feasible. The protocol and feasibility findings have been written up as a chapter in my final thesis that will be submitted later in 2020.
To supplement the clinical study, existing tissue samples from an animal study investigating post-traumatic OA (PTOA) were evaluated for gene expression and histological disease severity to understand the relationship between the IFP and the other structures within the joint including the synovium. As part of this project, we developed a novel instrument to evaluate sub-synovial fibrosis in the murine model. This work has resulted in three chapters of the final theses (1. Methods, 2, IFP and synovium, 3, IFP and other structures) and will be incorporated into a bigger manuscript for submission on which I will be a co-first author.
Between April 2019 and February 2020, I also carried out a systematic review and meta-analysis evaluating the relationship between IFP inflammation and pain in pre-clinical and clinical studies in the current literature. The manuscript for this study (which is also a chapter) is being revised before re-submission. In January 2020, I also commenced a study evaluating the same relationship in a publicly available database: The Osteoarthritis Initiative. This manuscript (and chapter) is currently under peer-review with the Osteoarthritis and Cartilage Journal.
I also was the winner of the Musculoskeletal Centre for Research Excellence Infographic Competition with my entry entitled “5 Things you need to know about the IFP and OA”.
Psoriatic Arthritis – An observational & longitudinal study
| Funded by: | ARA VIC Fellowship |
| Recipient: | Anna Antony |
| Intended Department | Rheumatology- Monash University |
| Project: | Longitudinal Psoriatic Arthritis observational cohort study |
The intention of this project was to establish a second parallel psoriatic arthritis clinic at Monash Health, in which annual reviews of patients could be undertaken to collect longitudinal data that should provide important data regarding the natural history, treatment responses and impact of disease on an Australian cohort of PsA patients, as well as to prospectively investigate the prevalence and incidence of common metabolic co-morbidities such as hypertension, dyslipidaemia, obesity and non-alcoholic fatty liver disease.
Following the receipt of the grant, a business case was put forward for the clinics and the clinic was approved for commencement at the end of the first quarter of 2020. Working relationships were fostered with the gastroenterology department to facilitate regular fibroscans, a non-invasive test for fatty liver disease. An ethics submission for data collection was submitted and provisionally approved by research governance at Monash Health. Unfortunately, the COVID-19 pandemic halted the commencement of any new clinics just prior to our project getting underway.
I expect to be able to provide a final report with outputs that are relevant to the fellowship in 12 months.
Spondyloarthropathy- Evaluating responses to infection and inflammation
| Funded by: | Fellowship Queensland’s Allen and Gwen Warren Fellowship |
| Recipient: | Tommy (Xiao) Liu |
| Intended Department | University of Queensland Diamantina Institute |
| Project: | Evaluating how Endoplasmic Reticulum stress augment responses to bacterial infection and inflammation in a mouse model of spondyloarthropathy. |
My research focus is Spondyloarthropathy (SpA), a group of autoimmune diseases that includes reactive arthritis (ReA), ankylosing spondylitis, psoriatic arthritis (PsA), and arthritis associated with inflammatory bowel disease. This group of conditions is characterised by inflammation of the spine (spondylitis), large joints and entheses (connective tissue between tendon or ligament and bone), skin (psoriasis), and ileitis or colitis. Interestingly, studies have identified common genetic links between individuals who develop different manifestations of SpA, which are linked to cellular stress, enhanced inflammatory responses, and reduced control of bacterial infections. My research aims to uncover the initial events that lead to abnormal immune responses manifesting as disease in genetically susceptible individuals.
This project focused on the ability of bacterial infections to exploit elevated cellular stress in susceptible hosts, which lead to chronic inflammation and disease development. Using a preclinical model of ReA, I highlighted a key role for macrophages, a type of white blood cell, to take up and disperse Chlamydia from the genital tract to other tissues after infection. Inflammatory arthritis and skin disease were dramatically suppressed when macrophages were depleted, which was associated with reduced inflammation and cellular stress. Furthermore, I have shown a relationship between cellular stress and the severity of SpA. In mice resistant to cellular stress, clinical signs of PsA were markedly reduced, which was associated with reduced markers of inflammation.
Standard SpA treatments begins with non-steroidal anti-inflammatory drugs and conventional Disease-modifying anti-rheumatic drugs (DMARDS) which are effective in suppressing disease activity and slowing progression in Rheumatoid Arthritis, but are less successful in patients with SpA, especially those with spinal disease. Biological DMARDS such as Tumour Necrosis Factor inhibitors are limited by adverse events and failure to respond while rarely achieving drug-free remission. These approaches target and alleviate inflammation but ignore the underlying mechanisms of disease, including cellular stress, abnormal gut microbiome, and compromised control of bacterial pathogens.
The overarching question my grant set out to answer was whether limiting cellular stress will improve host defence against bacterial infections and reduce the severity of psoriatic arthritis and reactive arthritis in preclinical models. More specifically, I aim to discover whether enhanced cellular stress in individuals affect mucosal barrier integrity in the gut (in psoriatic arthritis) or genital tract (in reactive arthritis), which impairs normal host defence against bacterial infections. Elevated cellular stress in the hosts’ immune system may negatively affect the ability to clear bacterial infections, resulting in the activation or persistence of inflammatory pathways that drive disease development/progression.
Answering these questions will fill current knowledge gaps in the factors that drive SpA development in susceptible individuals in addition to the conditions, which lead to clinical relapse upon treatment cessation. Addressing these questions will highlight the mechanisms that drive inflammation, providing a therapeutic strategy to alleviate cellular stress and improve mucosal integrity to prevent disease development and/or reduce disease severity.
In ReA, one of the key unanswered questions is how arthritis manifests from infections in the genital tract. My findings have demonstrated that after Chlamydia infection, macrophages recruited into the genital tract take up and disperse Chlamydia to other tissues. Additionally, in mice susceptible to SpA, macrophages display reduced ability to clear bacterial infections and therefore elevating overall bacterial burden. The link between macrophages and clinical manifestation of disease is highlighted further with a dramatic reduction in joint disease when macrophages were depleted before Chlamydia infection. This observation was associated with increased cellular stress and production of mediators of inflammation in the genital tract and joints. Furthermore, immune cells isolated from cellular stress resistant mice after Chlamydia infection produced lower levels of proinflammatory factors than controls. Together, these findings identify the pivotal role played by macrophages in ReA and highlight cellular stress as a potential therapeutic target.
In PsA, I demonstrated that mice resistant to cellular stress develop less severe psoriatic arthritis. I have focused on two potential factors that may have contributed to decreased disease severity 1) improved gut barrier integrity and 2) enhanced immune control of bacterial infections.
There is strong association between gut inflammation (also known as leaky gut syndrome) and SpA. The intestinal barrier plays a key role in interacting with beneficial bacteria and keeping potentially harmful bacteria at bay. Physical disruption or impairment of the integrity of the gut barrier due to elevated cellular stress may result in bacterial infections and over-activation of proinflammatory responses by the host immune system. To test this, control mice and mice lacking a key gene mediating cellular stress (CHOP) were orally administered the molecule FITC-dextran. One and four hours after treatment, lower levels of FITC-dextran were detected in the blood of cellular stress resistant mice compared to controls This result indicated that reduced cellular stress improved gut barrier integrity and reduced leakage of FITC-dextran from the gut into the blood stream.
Impaired immune control of bacterial infections is another explanation of how SpA develops in susceptible individuals. One of the major immune cells responsible for bacterial clearance is the macrophage, which eat and rapidly kill bacteria by producing antimicrobial factors. However, some forms of bacteria such as Salmonella can exploit elevated cellular stress in macrophages and enter a dormant and persistent state. This results in the macrophages producing excessive pro-inflammatory factors, such as TNF leading to disease manifestation. My results have shown that the immune systems of mice resistant to cellular stress produce more bacteria-clearing inflammatory factors and less SpA-associated mediators. Whether this translates to an improvement in the capacity of macrophages to kill bacteria requires further investigation. Nonetheless, these results demonstrate the relationship between cellular stress, gut integrity, and immune control of bacterial pathogens.
The findings of my research are still preliminary but may benefit people with musculoskeletal disease in the future. Exploring how cellular stress and impaired control of bacterial infections contribute to inflammatory processes that lead to disease development will benefit future research into novel treatments for SpA and other autoimmune diseases such as Rheumatoid Arthritis.
If my hypotheses are correct, the next step is to deliver antibiotics or inhibitors of cellular stress to macrophages or to the mucosal barrier to facilitate bacterial clearance and/or improve barrier integrity. This would be expected to prevent disease development in people at risk and to suppress clinical signs of psoriatic arthritis and reactive arthritis in people with disease.
Shoulder pain study - choosing between non-surgical treatment or surgery.
| Funded by: | Arthritis Australia |
| Recipient: | Joshua Zadro- GIA |
| Intended Department | Sydney School of Public Health, Faculty of Medicine and Health, The University of Sydney |
| Project: | The development of a patient decision aid to reduce subacromial decompression |
We interviewed 26 health professionals (11 physiotherapists, 7 orthopaedic surgeons, 4 general practitioners, 3 chiropractors and 1 osteopath) and 14 people with shoulder pain to help us develop a decision-making tool to help people with shoulder pain choose between non-surgical treatments (e.g. exercise) and shoulder surgery.
Shoulder pain affects up to 1 in 4 people at any given time. Two surgeries are often performed for people with common causes of shoulder pain like rotator cuff tears and impingement; subacromial decompression surgery and rotator cuff repair surgery. Recent high-quality scientific research suggests subacromial decompression surgery provides no more than a placebo effect and rotator cuff repair surgery is not superior to non-surgical treatments, such as exercise and activity modification. Despite this, use of subacromial decompression surgery and rotator cuff repair surgery has doubled in Australia since 2001 (7,455 subacromial decompression surgeries and 12,436 rotator cuff repairs were performed in 2019).
Decision-making tools that present evidence on the benefits and harms of different treatment options can improve patients’ knowledge and satisfaction with decision-making and reduce use of unnecessary treatment. We developed a decision-making tool to help people with shoulder pain make an informed choice between non-surgical treatments (e.g. exercise) and surgery. Interviews highlighted agreement among health professionals and people with shoulder pain on most aspects of the decision aid (e.g. treatment options, summary of benefits, harms and practical issues, questions to ask a health professional, graphics, formatting). However, some aspects of the decision aid elicited divergent views among health professionals (e.g. causes and symptoms of shoulder pain, evidence on benefits and harms). This decision aid could be an acceptable and valuable tool for helping people with shoulder pain make informed treatment choices. A randomised controlled trial evaluating whether this decision aid reduces people’s intentions to undergo shoulder surgery and facilitates informed treatment choices is underway.
By eliciting the views of people with shoulder pain and health professionals, the aim of this project was to develop a decision-making tool that presents un-biased scientific information on the benefits and harms of shoulder surgery (e.g. subacromial decompression surgery and rotator cuff repair surgery) and non-surgical treatments for people with shoulder pain.
Previous research has demonstrated the benefits of decision-making tools for a variety of conditions. Decision-making tools help patients make informed choices about their healthcare, with no negative effects on their health or satisfaction with care. Once patients are informed of the benefits and harms of their options, they often choose more conservative (or less invasive) options.
We have developed the first decision-making tool people with shoulder pain considering surgery. Given the increasing rates of subacromial decompression surgery and rotator cuff repair surgery in Australia and globally, this tool could help patients make informed decisions and reduce the use of these surgeries.
By eliciting views of key stakeholders, we developed a patient decision aid that presents evidence-based information on the benefits and harms of subacromial decompression surgery and rotator cuff repair surgery for subacromial pain syndrome compared to non-surgical options. Most health professionals and people with shoulder pain rated all aspects of decision aid usability as adequate-to-excellent (e.g., length, amount of information, presentation, comprehensibility).
Interviews highlighted agreement among health professionals and people with shoulder pain on most aspects of the decision aid (e.g. treatment options, summary of benefits, harms and practical issues, questions to ask a health professional, graphics, formatting). However, some aspects of the decision aid elicited divergent views among health professionals (e.g. causes and symptoms of shoulder pain, evidence on benefits and harms).
Highly consistent feedback included praise for including the practical issues of surgery and non-surgical options (e.g. time off work, anaesthetic) and a global summary of the benefits and harms of each, and praise for including a section on ‘questions to ask a health professional’. Health professionals and patients largely agreed with the presentation of non-surgical and surgical options, with some patients pleased to have ‘wait and see’ included as this aligned with their experience of pain that has resolved without treatment. Most health professionals and patients wanted non-surgical options listed before surgery to mimic treatment recommendations in real-life.
We found quite varied feedback on the causes and symptoms of shoulder pain and presentation of benefits. Most health professionals and patients thought the causes and symptoms of shoulder pain were accurate and easy to understand. However, some health professionals (mostly physiotherapists) thought the description of shoulder pain was inappropriate and used language that could cause fear and drive patients towards surgery. Some orthopaedic surgeons disagreed with the evidence we used on the benefits and harms of surgery, and thought the decision aid was biased against surgery. On the other extreme were some physiotherapists, who suggested that the same evidence underestimated the true harms of surgery.
Nearly 3 in 4 patients thought the decision aid was biased against surgery, likely because the evidence we presented shows subacromial decompression surgery and rotator cuff repair surgery are not superior to non-surgical management. This suggests tools for assessing perceived balance of decision aids may not be suitable when a decision aid presents information that counters prevailing norms.
You can read more about this project here: Scientific Summary- Dr Zadro
Personalised Medicine in the Treatment of Ankylosing Spondylitis
| Funded by: | Arthritis WA and Arthritis QLD |
| Recipient: | Assoc Prof Tony Kenna |
| Intended Department | Institute of Health and Biomedical Innovation-Queensland University of Technology |
| Project: | Personalised Medicine in the Treatment of Ankylosing Spondylitis |
Ankylosing spondylitis, or AS for short, is a form of arthritis that affects joints in the spine and pelvis, causing them to fuse together which results in severe pain and disability. The immune system plays an important role in AS and we know that drugs that shut down or inhibit parts of the immune system provide considerable symptom relief to patients including relief of pain. Until recently there were very few of these drugs available and patients were typically treated with the drug that best suited their clinical symptoms. However, new families of drugs are now available with more in development and the selection of which drug to use on which patient needs now to be better informed and to include an understanding of the patients’ immune profile. Our project studied groups of AS patients who have either responded well or poorly to treatment with two of these families of drugs, anti-TNF or anti-IL-17 monoclonal antibodies, to determine whether there are tell-tale ‘signatures’ in their immune or genetic profiles that could have predicted their treatment response.
We developed a sophisticated assay to study patient immune cell functions in detail. This uses a technique called flow cytometry which allows us to measure amounts of protein expressed in and on cells. Our flow cytometry assay has been designed to measure 28 key proteins that regulate immune cell functions. This assay was the applied to patient samples. The patients were selected from a biobank and were chosen as patients who had previously responded poorly to anti-TNF drugs and subsequently responded well to anti-IL-17 therapy. A second group of patients who responded well to anti-TNF treatment was also studied. In parallel measured expression of immune genes using a technique called RNA-sequencing. From our flow cytometry analysis we were able to determine an immune signature that segregates with patient drug responses. Analysis of our gene expression study is complex and will require further study to unlock its full potential. Overall, this pilot study suggests that study a patients immune cells may be an effective way of tailoring treatment options for AS.
You can read more about Tony Kenna’s project here: Scientific Report- Assoc Prof Tony Kenna
Rheumatology- research on the impact of ongoing medication adherence
| Funded by: | Marion A Simpson Grant |
| Recipient: | Dr Ayano Kelly |
| Intended Department | Medical School-Australian National University |
| Project: | Outcomes of adherence interventions in rheumatology |
Taking medications as prescribed (i.e. medication adherence) is challenging for many people living with chronic health conditions such as rheumatic conditions. Many people living with inflammatory rheumatic conditions (including rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, lupus, gout and osteoporosis) need to take life-long medications to relieve symptoms, prevent long term joint and organ damage and improve daily activities. Despite an increasing number of strategies (or “interventions”) that have been tested to support medication adherence for patients with rheumatic conditions, many of these have not been shown to work. It is important that these studies are designed so that they evaluate results (also known as outcomes of a study) that are meaningful to patients and health professionals, and feasible to use by researchers.
Our research group has conducted multiple studies with a goal of improving future research testing different adherence interventions, including a review of existing studies aiming to improve medication adherence in rheumatology and an Australian focus group study that asked patients and caregivers with gout, osteoporosis and rheumatoid arthritis to discuss what they felt impacted their medication adherence. Building on this previous work, we were able to do international focus groups in Australia, Netherlands and Canada to understand what results or outcomes would be important to patients, if they were to be supported with medication adherence, this helps to identify a core set of outcomes of adherence interventions from a patient’s perspective.
In addition, to capture the perspectives of stakeholders that are experts in conducting and evaluating adherence interventions, interviews were conducted with international medication adherence researchers. Information gathered in these activities will be used to develop a multi-round online Delphi survey that will be sent to patients, caregivers, health professionals, researchers and others to get agreement on a core set of outcomes to be used in adherence intervention studies. Our overall goal is to improve the design of studies testing interventions aimed to improve medication adherence in rheumatology, so that they evaluate and ultimately improve outcomes that are consistent, and important particularly to patients and the health professionals who help manage them.
The questions we set out to answer with this grant were:
- To describe international patients’ perspectives on the design and evaluation of adherence intervention studies (Study 1).
- To describe adherence researchers’ perspectives and experiences on the design and evaluation of adherence intervention studies (Study 2).
We are also using the results of these two studies to design a further study:
- To generate a consensus-based prioritised list of core outcomes for trials testing adherence strategies in rheumatology (Study 3).
We conducted Study 1 as we wanted to gain insights into what patients value as outcomes of adherence interventions. To the best of our knowledge, patients have never been systematically asked to provide input into this aspect of adherence research design in any medical field. We conducted Study 2 as medication adherence research is an emerging field in Rheumatology, and we wanted to describe the perspectives of experienced adherence researchers. We believe Study 2 is also novel, and provides key insights to advance this field of research forward in Rheumatology. Overall both studies are important in order to design studies to support patients with their medication adherence, so that it addresses the outcomes that are of importance to patients, using the advice and knowledge of experts in the field.
Study 1 – Patient perspectives on outcome domains of medication adherence trials in inflammatory arthritis: an international OMERACT focus group study
Adult patients (≥18 years) with inflammatory arthritis using disease-modifying anti-rheumatic drugs (DMARDs) from centres across Australia, Canada, and the Netherlands participated in six focus groups (38 participants) to discuss outcome domains of medication adherence trials that they consider important. Improved outcome domains that patients would want from participating in an adherence trial were categorised into five types: medication adherence, adherence-related factors (e.g. medication knowledge), pathophysiology (e.g. physical functioning), life impact (e.g. ability to work), and economic impact (e.g. productivity loss). Three overarching themes reflecting why these outcome domains mattered to patients were identified. First, how taking medications could improve patient’s emotional and physical fitness to maintain their social function. Second, how improving knowledge and confidence in self-management increase patient’s trust in and motivation to take medications as agreed with minimal risk of harms. Finally, how respect and reassurance, reflecting healthcare that values patient’s opinions and is sensitive to patient’s individual goals could improve medication taking behaviour. Patients value various outcome domains to be evaluated in future adherence trials related to their overall well-being, confidence in medication use and patient-healthcare provider relationships.
Study 2 – Researchers’ perspectives on methodological challenges and outcomes selection in interventional studies targeting medication adherence in rheumatic diseases: An OMERACT-Adherence international qualitative study
Semi-structured interviews using audio conference were conducted with 13 researchers from seven countries, who had conducted an adherence study of any design in the past 10 years. We identified three themes: 1) improving measurement of adherence (considering all phases of adherence, using appropriate and relevant measures, and establishing clinically meaningful thresholds); 2) challenges in designing and appraising adherence intervention studies (considering the confusion over a plethora of outcomes, difficulties with powering studies to demonstrate meaningful changes, and suboptimal descriptions of adherence interventions in published studies); and 3) advancing outcome assessment in adherence intervention studies (capturing rationale for developing a core domain set as well as recommendations and anticipated challenges by participants). Gathering perspectives from international adherence researchers, our findings led to researcher-informed recommendations for improving adherence research including specifying the targeted adherence phase in designing interventions and studies and providing a glossary of terms to promote consistency in reporting. We also identified recommendations for developing a core domain set for interventional studies targeting medication adherence including involvement of patients, clinicians, and other stakeholders and methodological and practical considerations to establish rigor and support uptake.
Both study 1 and 2 are complete. Study 1 has had minor revisions and a resubmission for publication in a peer-reviewed journal, study 2 has been accepted for publication by the BMC Rheumatology journal. We are hoping that with further dissemination of these results, more research will continue in Rheumatology to support patients with medication adherence, and consider the values and perspectives of patients, and advice from medication adherence research experts.
We are using the results of all our previous research to design a Delphi survey. We have created a draft video (Click here to view) to introduce the survey to patients, and other participants. We have been accepted for the 2022 OMERACT conference to move to the final steps of this research.
Targeting treatment of inflammatory Rheumatoid Arthritis - A therapeutic option
| Funded by: | Marion A Simpson Grant |
| Recipient: | Dr Cynthia Louis |
| Intended Department | Inflammation Division-The Walter and Eliza Institute of Medical Research – (WEHI) VIC |
| Project: | Targeting specific cell survival proteins to treat inflammatory arthritis |
We have a longstanding interest in research on Rheumatoid Arthritis (RA) and related rheumatological diseases. Despite recent treatment advances, many patients do not respond to current therapies and sustained disease remission is still rare. To address this problem, our current projects focus on new immune and inflammatory pathways that drive arthritis. Ultimately, we hope to translate research into the clinic to benefit patients. Funding from Arthritis Australia has allowed us to investigate how joint inflammatory cells can be selectively targeted in a preclinical model of arthritis. Results from this study offer a new therapeutic option for consideration in RA but also other inflammatory joint diseases.
Abnormal cell survival can cause cancers but also contribute to chronic inflammation in diseases such as RA. WEHI has been at the forefront of research to understand the molecular pathways governing cell survival and cell death. A suite of molecular targets have been identified and antagonists have been developed. Recently, this research led to the introduction of Venetoclax as a new treatment for leukaemia. The grant set out to identify how inflammatory cells persist in arthritic joints and whether existing drugs that target pro-survival proteins can be similarly used to alleviate joint inflammation while maintaining cells in other organs. This is important because current drugs for RA can deplete immune cells outside the inflamed joints, leading to compromised immunity in patients.
Chronic inflammation in RA is characterised by the recruitment of inflammatory immune cells from the blood into arthritic joints. One of these cells are called neutrophils. They are known to drive joint inflammation by producing noxious factors. Once neutrophils enter affected organs, they need to undergo regulated cell death to prevent ongoing inflammation. Failure to do so can lead to progressive joint damage and prevent tissue healing, such as the case in RA joints. Therefore, we believe strategies that can reduce neutrophil numbers specifically within the inflamed joints will alleviate arthritis and minimise joint destruction. We confirmed that inflammatory signals can extend the survival of neutrophils. We also found that this is mediated by specific cell survival protein called BCL-XL. We found that blocking the pro-survival molecule BCL-XL can prevent the development of severe arthritis in a preclinical arthritis model. Specifically, BCL-XL antagonist (a drug that blocks BCL-XL) significantly reduces joint neutrophil numbers without affecting neutrophils in other organs. These results demonstrate the therapeutic potential of BCL-XL antagonist in inflammatory joint diseases without compromising immune cells in other organs. Given the preclinical nature of this project, the findings have not benefitted patients with musculoskeletal disease. However, results from these studies are encouraging, paving the way towards further proof-of-principle studies and clinical trials. We have revealed BCL-XL as a mechanism by which inflammatory cells (i.e. neutrophils) persist in inflamed organs and propagate tissue destruction. Subsequently, we also show that blocking this survival node with BCL-XL antagonist not only prevents the development of severe inflammation in arthritis model, but also other inflammatory settings such as sepsis and lung inflammation. These results suggest that BCL-XL antagonists may be therapeutically applicable in many other debilitating inflammatory diseases driven by neutrophils, including sepsis, chronic obstructive pulmonary disease and gout. In a small set of experiments, the BCL-XL antagonist could also kill inflammatory neutrophils taken from the inflamed joints of arthritis patients. This confirms the clinical efficacy and supports the therapeutic potential of BCL-XL antagonist to treat several human diseases. Another known effect of BCL-XL antagonists is their propensity to reduce platelet numbers (thrombocytopenia). This is because platelets, tiny cell fragments responsible for blood clotting, require BCL-XL to survive. While this condition may be a concern and a preference would be to prevent drug-induced thrombocytopenia altogether, having reduced number of platelets may in fact offer an additional therapeutic benefit in chronic inflammatory syndromes. Our future research is focused on developing new BCL-XL antagonists that spare platelets and examine whether they similarly block inflammatory arthritis and if they can be applied to other inflammatory diseases where therapeutic options remain limited.
You can read more about this project here: Scientific Report – Dr Cynthia Louis
Hip Osteoarthritis - In depth study on walking and its effects
| Funded by: | Eventide Homes |
| Recipient: | Dr Laura Diamond |
| Intended Department | School of Allied Health Sciences-Griffith University |
| Project: | Personalised hip joint load modification using real-time biofeedback |
Rates of total hip replacement are spiralling upwards in Australia, highlighting the urgent need to improve current evidence-based treatment options for hip osteoarthritis (OA). Conservative non-drug interventions are recommended for management of hip OA, though many patients report only small-to-modest improvements in symptoms. This may be because treatments are largely based on evidence from knee OA literature. Lower hip loading has been implicated in the progression of hip OA and is potentially modifiable with movement retraining. The proposed study tested the extent to which hip loading could be normalised by changing the way people with hip OA walk – in real-time. We integrated our newly developed real-time biofeedback technology to personalise and enhance motor learning and tested sustained effects for symptoms after 6-weeks. We also sought feedback from participants regarding their comfort when walking over the 6-week period, perceived change in biomechanics and pain, and acceptability of personalised load modification as a treatment for hip OA.
Twenty people with mild-to-moderate hip OA participated in the study. Biomechanics and patient-reported data were collected at baseline and patient-reported data were collected at 6-week follow-up. Most participants with hip OA could immediately increase their hip load through personalised movement retraining by an amount expected to stimulate cartilage heath and reported an improvement in symptoms after 6-weeks. However, the hip’s load response to each modification was unique across participants, emphasising the need for personalised interventions for management of hip OA.
Conservative treatments for hip OA are cost-effective, yet they are under-used, have unsatisfactory outcomes, and do not alter the disease-course. We aimed to design and test a new disease-course altering treatment for hip OA. We used a within-participant design to compare the feasibility of three biomechanical parameters for increasing hip load when participants were provided with real-time visual biofeedback during walking, and prospectively evaluated any associated changes in pain and function 6-weeks following personalised retraining. We have shown, for the first time, that people with hip OA can increase hip load by as much as 12% through movement retraining with assistance from visual biofeedback. We have also identified which biomechanical parameters are most effective for modulating hip load, and critically, shown that many patients who implemented their personalised load modification strategy while walking for 6-weeks reported clinically important improvements in hip pain and function. Results from this pilot study support the feasibility of personalised hip loading retraining using real-time biofeedback technology for management of hip OA.
The study aimed to design and test a new disease-course altering treatment for hip OA by evaluating (1) the extent to which hip load could be modulated by changing external biomechanical parameters with assistance from real-time biofeedback during walking in people with hip OA; (2) which biomechanical parameter(s) were most effective for increasing hip load in people with hip OA; (3) associated changes in pain and physical function following 6-weeks of walking using a prescribed personalised load modification strategy in people with hip OA; and (4) the extent to which people with hip OA considered personalised load modification a feasible and acceptable treatment.
We discovered that (1) hip load could be increased by up to 12% through movement retraining with assistance from visual biofeedback in participants with hip OA – this finding is particularly significant because increasing joint load by even 5% may be enough to stimulate cartilage health; (2) two of the biomechanical parameters we assessed were equally effective for increasing hip load in participants with hip OA; (3) most participants with hip OA reported clinically meaningful improvements in hip pain and function after 6-weeks of walking using their prescribed personalised load modification strategy; and (4) the majority of participants with hip OA were confident when walking using their personalised load modification strategy.
Patient-centred stakeholders have demanded non-surgical and non-drug treatments, including biomechanical strategies, be a top OA research priority. The most frequently asked question by people with hip OA is “What can I do myself to decrease symptoms?”. We combined our novel technology with extensive scientific and clinical expertise to design and test a new biomechanical treatment which, unlike currently available options, has potential to alter the disease-course. Study findings confirmed that people with hip OA can modify hip loading through personalised laboratory-based retraining. Next, we will design a well-powered study to establish the extent to which hip load must be increased to be associated with a clinically meaningful improvement in symptoms.
We plan to move outside the laboratory by designing smart technology to provide continuous real-time reinforcement of beneficial hip loading strategies during activities of daily living to people with hip OA. Moving outside the laboratory will empower people with hip OA to self-manage their condition and drive their own improvements in symptoms. In the future, this conservative management strategy will have great potential to significantly advance patient management, clinical practice and policy, and substantially reduce health care costs.
You can read more about this project here: Scientific Summary-Dr Laura Diamond
An Investigation of the Variations in Knee Replacement for People with Osteoarthritis in Australia
| Funded by: | Australian Rheumatology Association (ARA) |
| Recipient: | Dr Yingyu Feng |
| Intended Department | Institute of Bone & Joint Research, Rheumatology Department-University of Sydney, Royal North Shore Hospital |
| Project: | Improving health outcomes through appropriate care: An Investigation of the Variations in Knee Replacement for People with Osteoarthritis in Australia |
OA affects one in eleven Australians and is the leading cause of disability. It is crucial to provide appropriate care for this large population. In Australia, 98% of knee replacements are attributable to pain and mobility problems associated with osteoarthritis (OA). The rate of total knee replacement (TKR) was one of the highest in the world; it also varies substantially by areas. Some of the variations may not be related to patients’ needs or preferences, or unwarranted variation. Unwarranted variation raises concerns about equity and appropriateness of care. To reduce the potential harms and inappropriate patient care for people with OA, we must identify unwarranted variation, understand the contexts influencing utilisation and contributing factors in order to properly address the problem and reduce inappropriate care.
Our research is the first Australian-wide study that investigates contexts influencing utilisation and contributing factors to geographical variation in TKR surgeries, taking into the local health demand or healthcare supply contexts. Understanding these factors holistically is an important step to reducing inappropriate use of TKR and optimising orthopaedic care to people who are in genuine need. The evidence derived from the research has a direct impact on the appropriateness levels and quality of OA care and contributes to the development of overuse of TKR by people with OA.
Our research explored the magnitude of the variation between local government areas (LGA), a much more granular geographical scale than what has been investigated in the current literature. We hope to understand where, for whom, and why the rates of knee replacement vary, and provide evidence for optimal approaches to responding to variation in TKR.
We found that there was a significant variation in TKR at the LGA level and people living in areas with higher arthritis prevalence and higher surgeon density received more TKR. The evidence suggests that demographic patterns and disease prevalence in the local areas have great implications for predicting and planning OA service needs.
The grant aimed to investigate the magnitude of and associated drivers for variation in TKR surgeries in Australia. There is currently relatively little research in the existing literature and hence a lack of evidence supporting the best methods or models to respond to the TKR variation. The variation in TKR revealed in the Australian Atlas of Healthcare Variation Series was at a very broad regional level and did not investigate the potential drivers. Measuring variation and investigating the contributing factors are important steps to reduce inappropriate use of knee replacement. Previous methods to improve OA service delivery have largely focused on changing individual clinician and patient behaviour, but strategies targeting specific regions to implement change may be more efficient.
We found that the TKR rate for OA in Australia was one of the highest in the world (227.1 per 100,000 population), more than double the rate in New Zealand (111 per 100,000). There is a significant variation across LGAs in Australia: over 30-fold difference between the highest and lowest areas, after the exclusion of the highest and lowest 10%. We also found that older Australians, areas with higher arthritis prevalence rates and higher density of orthopaedic surgeons had higher TKR utilisation rate. This suggested that inequalities in the utilisation of TKR were associated with local demographics, health needs and service supplies.
We also hypothesized that areas with high socioeconomic status, higher private health insurance and higher prevalence of obesity, one of the important risk factors for OA, may have high TKR rates. However, this is not the case when we adjusted patients’ age and sex within their local LGAs. There remained a significant variance in TKR utilisation after considering all the factors investigated in our research, suggesting other factors, relating to individual patients, surgeons or hospitals also contribute to the variations in TKR. It is important to establish whether provision matches actual need across socio-demographic groups to determine potential areas of service inequity across the country, which is what we plan to extend the research in the future.
This is the first Australian-wide study that investigates factors associated with variation in TKR surgeries at a small geographical scale. By examining patterns of OA and hence the demand for TKR, we can understand where unwarranted variation in TKR and potentially inappropriate care are provided for people with OA. The research is not only necessary but also timely for health policymakers to take actions to ensure right treatments and health services are provided to and accessed by the right people in the right areas, and thereby enhance health outcomes for people with OA in Australia.
We investigated variations between patient residential areas in the current research and plan to extend the research in several ways. We will improve the measurement for orthopaedic care supply through GIS approaches to measuring distance-to-surgeon GIS approaches. Additionally, we plan to examine variations between hospitals, taking into care supply factors. This will provide a clearer and more complete picture on the variation from both where patient lives and where they undertake surgeries, so as to ensure service provision matches actual need across socio-demographic groups in the local areas across the country.
You can read more about this project here: Scientific Summary- Dr Ying Yu Feng
Osteoarthritis - an investigation in pain management
| Funded by: | Reckitt Benckiser (Nurofen) Grant and Arthritis Australia |
| Recipient: | Dr Feng Pan |
| Intended Department | Menzies Institute for Medical Research-University of Tasmania |
| Project: | The role of systemic inflammation in osteoarthritis pain trajectories |
Osteoarthritis (OA) is the most prevalent form of arthritis in Australia and worldwide. OA is a chronic and painful disease of the synovial joint, and a leading cause of disability. Knees, hips and hands are the most commonly affected joints. Pain is the most prominent symptom which drives patients to seek healthcare. Thus, OA represents an enormous health and economic burden on patients and societies. There were 100,000 knee and hip replacement procedures (mainly due to OA) performed in Australian hospitals during 2015, with a cost of $2 billion a year. Despite this, there are no proven strategies to prevent, slow, halt or reverse the OA progression. Current OA management is mostly palliative and focuses on pain relief. ‘First-line’ agents, such as paracetamol and non-steroid anti-inflammatory drugs (NSAIDs), have only small to moderate efficacy, with >75% of patients reporting the need for additional symptomatic treatment. Therefore, pain control remains a substantial unmet need for OA treatment. In addition to the need to develop drugs that can slow disease progression, there is a critical need to develop more effective pain relief agents for OA patients.
Current ‘one size fits all’ approach in OA management and ongoing clinical trials and lack of in-depth understanding of the mechanisms of OA structural damage and pain explain the overall lack of treatment efficacy and frequent negative findings from OA clinical trials. OA is a heterogeneous condition characterised by a complex and multifactorial nature. With the increasing understanding of OA risk factors and pathological processes, it has become clear that OA is not only a disease of cartilage but it can be divided into different clinical phenotypes (e.g. chronic pain-, inflammatory-, bone- phenotypes). This leads to a large variation in clinical presentations (pain) and responses to OA treatment. Therefore, in order to optimise treatment effects in OA, the ‘one size fits all’ treatment approach needs to change to more tailored interventions targeting specific subgroups/phenotypes.
My research primarily focuses on the identification of biomechanical risk factors for chronic pain and OA, identifying OA pain subgroups/phenotypes and testing new therapeutic strategies based on phenotyping. I have identified distinct OA pain subgroups using advanced statistical methods. These subgroups differ in the underlying causes and mechanisms and consequently may require different therapeutic approaches. My research findings have contributed to a paradigm shift in the understanding of the pathogenesis of OA and OA-related pain.
Pain experience in knee OA is individualised and complex. Inflammatory and metabolic pathways have been suggested to play a key role in the pathophysiology of osteoarthritis-related pain. Our recent studies demonstrate that pain in OA consists of homogeneous subgroups following distinct pain trajectories. Pilot data from a small sample found that inflammatory markers may be involved in the development and maintenance of worse pain trajectories. This project will expand our biomarker testing to a larger sample to determine the role of inflammatory and metabolic mechanisms in the development and maintenance of different pain presentations. This study will facilitate a comprehensive understanding of Inflammatory and metabolic mechanism in OA pain patterns, and , will also identify biomarkers that can define optimal patient populations for specific interventions, and have the potential to develop new therapeutic targets.
Multisite musculoskeletal pain (MSMP) is a common pain presentation. Musculoskeletal pain often occurs at multiple anatomical sites simultaneously with an estimate of 75% of adults aged ≥65 years having pain at multiple sites. Multisite musculoskeletal pain (MSMP) has a worse prognosis and a more detrimental impact on health outcomes than single-site pain. Experiencing MSMP is associated with poorer physical and mental health, poorer sleep quality, and increased risk of falls, and fractures, suggesting that MSMP could be a distinct disease entity.
Lipidomic profiling (including 850 lipid species) was performed in 536 participants from Tasmanian Older Adult Cohort Study (TASOAC) with assessments at baseline, 2.6-, 5.1- and 10.7-year. MSMP was measured by a self-reported pain questionnaire at four time-points and defined as painful sites ≥4; while serum samples for lipidomic profiling were only collected at the 2.6-year follow-up. Lipid concentrations were natural log-transformed. Persistent MSMP was defined if participants had MSMP at 2.6-, 5.1- and 10.7-year. The Benjamini Hochberg method was used for controlling for multiple testing. Among 536 serum samples, 530 passed quality control. Of these, there were 112 (21%) and 418 (79%) participants having persistent and non-persistent MSMP, respectively. Participants having persistent MSMP had a lower level of monohexosylceramide (HexCer) (d18:1/24:0 and d18:1/22:0), lysophosphatidylcholine (LPC) (18:2 [sn2], 18:1 [sn1]), and 15-MHDA [sn1] [104_sn1]) than those with non-persistent MSMP. In multivariable analysis with adjustment for age, sex, body mass index, physical activity, diabetes, total cholesterol, HexCer (d18:1/24:0 and d18:1/22:0), and LPC (18:2 [sn2], 18:1 [sn1]), and 15-MHDA [sn1] [104_sn1]) were significantly associated with persistent MSMP (OR ranging from 0.22 to 0.33, per log pmol/ml increase, p≤1.94×10-3) after controlling for multiple testing.
We are now examining the associations of lipids with other pain presentations such as pain trajectories, pain severity etc.
This research project will address an unmet clinical need for optimal pain management for patients with pain. OA is the most common form of arthritis and is the leading cause of pain and disability. With the growing aging population, along with the increase in obesity, OA has become a huge societal and economic burden in the developed world. Despite this, there are no effective disease-modifying OA drugs and the existing pain therapies have limited efficacy and a substantial risk of adverse events. OA pain is highly heterogeneous, with pain presentations varying among patients. Therefore, it is not surprising to see far disappointing results from “one-size fits all” treatment approaches in OA pain patients. Our research will directly address this need by identifying pain subgroups and providing an optimal patient selection tool. By using metabolomics to determine underlying mechanisms of different pain subgroups, we will also identify biomarkers that can define optimal patient populations for specific interventions, and have the potential to develop new therapeutic targets. This project will fundamentally change clinical pain management in patients with OA by selecting the right patients for the right treatment. This has significant benefits for families and communities to improve OA patients’ quality of life and save substantial healthcare costs in Australia and worldwide.
Our research will benefit all patients with OA pain, by addressing the heterogeneity of OA pain and its mechanisms. One of the most pressing needs in the health field is to select the right treatments for the right patients. This is a more pressing issue in the OA field, given the lack of effective disease-modifying OA drugs and limited efficacy of analgesics. A significant advance on improving the efficacy of current OA pain treatments would be a stratification method that can select patients who are most likely to respond to the treatments and minimise their suffering related to ineffective treatments. Based on our previously defined OA pain subgroups which differ in metabolic abnormalities and central pain processing, have different clinical health outcomes, and show a degree of phenotypic stability over time, this suggests that these pain subgroups are clinically useful in OA patients’ stratification. Researching metabolic mechanisms using metabolomics will better predict who will or will not benefit from a treatment, and who will or will not have the highest efficacy and the lowest safety concerns to a given treatment. Furthermore, the nature of cohort studies included in this project will enable the identification of mechanisms that underlie transition to and maintenance of OA pain. Therefore, this work will lead to a paradigm shift in our understanding of OA pain, and will lay the foundation for targeted treatments for patients with OA pain as well as other common and complex chronic pain conditions with similar pain mechanisms involved.
The outcomes of this project will advance scientific knowledge in revealing mechanisms of OA pain heterogeneity, and significantly improve the methods for stratifying OA pain patients. The project is multidisciplinary. It will provide new insights into OA pain mechanisms and treatments that will assist with developing an optimal and tailored therapeutic strategy for a selected subgroup of OA patients. Therefore, passing on the knowledge to other researchers, clinicians, and the wider community through communicating and disseminating our research findings is an important part of our research plan. We will publish the results of our research in top-tier journals and use high quality national and international pain and rheumatology conferences as a key part of the scientific communication chain. While data arising from our research lead to high impact and significant findings in academia, new biomarkers identified from this project may advance developing therapeutic products for Australia’s pharmaceutical industry to benefit more patients who are living with pain.
You can read more about this project here: Scientific Summary – Dr Feng Pan
Rheumatoid Arthritis (RA) – a study on the role of immune cells
| Funded by: | Arthrits Australia and the HJ & GJ McKenzie Grant |
| Recipient: | Prof Christopher Jackson, Meilang Xue, Lyn March and Lara Bereza-Malcolm |
| Intended Department | Sutton Arthritis Research Laboratory, Level 10, the Kolling Building, Royal North Shore Hospital, St Leonards NSW 2065 |
| Project: | Loss of EPCR attenuates inflammatory arthritis in mice via inhibiting DC maturation and migration |
Arthritis is the major cause of disability and chronic pain in Australia, and rheumatoid arthritis (RA) is one of the most damaging forms, with about 30 % of patients unable to work after 3 years of disease. RA is currently not curable. One of treatment strategies currently under development for this disease is to reinstate immune balance by selectively targeting a subset of immune cells named as dendritic cells. Manipulation of these cells has shown beneficial therapeutic effects in RA animal models and human RA patients. A receptor protein named EPCR has been found to be in high quantities in the RA joint where it attracts high numbers of mature dendritic cells, although the reasons behind this are unknown. This project investigated how EPCR modulates the function of two types of immune cells, dendritic cells and T cells, that play a critical role in RA using a mouse model of human RA.
For this study we used mice that had been genetically modified so they do not express EPCR (known as EPCR knockout mice). Our initial work revealed that these mice develop considerably milder arthritis when compared to control mice. Interestingly, we found that these knockout mice had higher numbers of dendritic cells in their blood, and the maturity of these cells varied markedly when compared to control mice. We also found that bone marrow and spleen cells derived from EPCR knockout mice were less likely to become inflammatory compared to normal cells and correspondingly, T cells from EPCR knockout mice produced less inflammatory molecules. These results help explain why EPCR knockout mice exhibit less severe arthritis compared to normal mice.
This grant set out to delineate potential links between EPCR, dendritic cells and T cells in RA, and how these cells associate with arthritis severity; and whether manipulation of EPCR affects inflammation in these immune cells and in RA.
We found overall dendritic cells were increased in blood, but decreased in peripheral lymph nodes; inflammatory T cells were low and anti-inflammatory T cells high in EPCR knockout mice in comparison to control mice; and that removal of EPCR dramatically affected the inflammatory response of dendritic cells..
This work is important because previously, we found that EPCR is over-presented in RA and promotes the destructive properties of RA synovial cells, but we have no direct evidence whether it contributes to RA. Discovery from this grant provides convincing and direct evidence showing that by removing this gene, the incidence and severity of arthritis is inhibited. Importantly, we found that this protein acts via modulating the function of dendritic cells. These findings support the basis of manipulating dendritic cells as a treatment strategy currently under consideration for RA.
We found that EPCR knockout mice develop considerably milder arthritis when compared to control mice. These knockout mice had higher numbers and more mature dendritic cells in their blood and in the synovial joints. Additionally, bone marrow and spleen cells derived from EPCR knockout mice were resistant to become inflammatory, even after being induced by known inflammatory mediators. When compared to control cells. After isolating T cells, EPCR knockout mice had more inflammatory T cells and less anti-inflammatory T cells compared to control mice. Correspondingly, cells from EPCR knockout mice produced less inflammatory mediators. These data indicate that the reduction in arthritis in EPCR knockout mice is likely achieved via modulating the inflammatory function of these specific immune cells.
Overall, this grant makes the discovery that EPCR is directly associated with RA onset and progression, and knockout of this gene inhibits the incidence and severity of arthritis. These functions of EPCR are achieved via modulating the function of dendritic cells. Modulation of these cells is one of the treatment strategies currently under development for RA. Our results suggest that a more specific approach involving EPCR may be a useful adjunctive therapy for RA.
This is a basic science research project and as such requires further work before it can directly benefit people with musculoskeletal disease.
We anticipate that our finding that EPCR can modify the function of dendritic cells will provide insights into the benefits of pharmacologically manipulating dendritic cell function via EPCR expression in RA patients and facilitate the development of innovative therapeutic interventions to prevent disease progression and improve the overall mobility of RA patients.
The next steps we plan to perform are:
- Detail the exact mechanisms of how EPCR modulates inflammation, focusing particularly on the immune cells.
- Test the therapeutic potential of manipulating EPCR using a mouse arthritis model.
A NHMRC grant application will be lodged to further these studies.
You can read more about this project here: Scientific Summary – Prof Chris Jackson
Sleep, pain and physical activity
| Funded by: | Australian Rheumatology Association (ARA) |
| Recipient: | Dr Tiffany Gill |
| Intended Department | Adelaide Medical School -The University of Adelaide |
| Project: | Sleep, pain and physical activity |
Pain due to musculoskeletal problems (such as osteoarthritis) has been shown to have a significant negative impact on sleep quality. In turn, both poor sleep quality and pain affect physical activity, likely restricting behaviour (movement), improving symptoms and quality of life in this patient group. However, the exact relationship between these three aspects has received limited attention. This lack of understanding means that we are unable to design interventions and provide targeted advice to encourage sleep and activity in patients experiencing pain associated with musculoskeletal problems.
This work extended a longitudinal cohort study in community-dwelling men. These participants have undertaken in-home sleep studies, and this study added musculoskeletal and physical activity data collection to determine the relationship between sleep, musculoskeletal pain and physical activity. The collection of comprehensive sleep data (using polysomnography) is expensive and time-consuming and is seldom performed in community samples. Therefore, this was a unique opportunity to improve further our understanding of sleep, musculoskeletal pain and physical activity. Through the addition of questions in a questionnaire and wearing a watch-like device on the wrist, we could get a more complete picture of how sleep, pain, and activity work together.
This project aimed to provide an improved understanding of the relationship between sleep, pain, and physical activity. Suppose the relationship between these factors is more precisely defined. In that case, it can lead to better designed, targeted interventions (precision care) to improve the management of patients living with pain associated with musculoskeletal conditions. There is the potential to increase activity, which is beneficial for musculoskeletal disorders and to improve sleep. If there are improvements in sleep, pain levels may also improve. These benefits would then improve the quality of life of people with musculoskeletal conditions.
Our work has indicated that while most men in the study did not do much physical activity, there was a wide range in activity levels. In addition, there were some differences in sleep patterns between men with and without pain. Those with high levels of exercise across the week day, also had high levels over the weekend. Some had lower levels during the week but had higher levels of weekend activity. Those with high pain levels also tended to have lower levels of activity. However, there were other participants with some level of pain who did undertake moderate/vigorous activity. There were also differences in time spent sleeping among those with and without pain. Other factors such as the location of pain, body mass index and depression also have a role to play.
More detailed analyses are being undertaken. These include the impact of medications and other co-morbidities. This information will be used to clarify the relationships further. Longitudinal analyses are also being undertaken to examine the associations over time with sleep, pain and activity.
The findings can be used in the future to provide an understanding of the relationships between sleep, pain and activity. Once this is understood, education and interventions can be designed to reduce musculoskeletal pain through improving sleep and activity levels and enhance the quality of life.
Once we have fully clarified the relationships, we will conduct intervention trials among people with musculoskeletal pain.
You can read more about this project here: Scientific Summary -Dr Tiffany Gill
Connect: Telecare health coaching management of low back pain in primary care
| Funded by: | Arthritis Western Australia and the Allan and Beryl Project Grant |
| Recipient: | Dr Manuela Ferreira/ Joanna Prior |
| Intended Department | Rheumatology Department-Institute of Bone and Joint Research
University of Sydney |
| Project: | Connect: Telecare health coaching management of low back pain in primary care. |
Approximately one in six Australians report low back pain at any one time, with 50% of the population reporting low back pain in the past month. This accounts for approximately $4.8 billion in Australia every year with direct health care costs. Low back pain is also the leading cause of disability world-wide with 540 million people globally affected by activity limiting low back pain. Key messages from the recent Lancet Series on Low Back Pain reveal that health care for low back pain is largely fragmented and poorly coordinated with most patients receiving low-value care that is not evidence-supported (e.g. opioids, routine imaging). A clear example of this practice is the high rate of presentations to emergency care for LBP. A recent analysis of consecutive ED visit charts in the USA identified over half of all presentations are for pain, of which 13% are for low back pain.
A recent study conducted in Australia showed that low back pain can comprise up to 2% of all ED presentations, with each ED presentation for LBP in Australia requiring an average of 4.5 hours of ED time, and costing tax-payers up to AUD2,5006. Our analysis of NSW Admitted Patient Data Collection also showed over 307,000 ED presentations for LBP in NSW between 2003 and 2012 (average of 30,000/year or AUD7.7million/year). There is also evidence that around one in five of these patients will represent6. ED representation rates for low back pain range from 12%6 to 19%7 creating a cycle of low-value care. Whereas most currently advocated models of care of LBP focus on ED admitted patient care, we lack evidence-based, integrated post-discharge monitoring. This fragmented and uncoordinated care leads to the high representation rates we have observed in EDs across Australia.
A common problem is that patients discharged from hospital may not adhere to adequate management. A promising way to facilitate behaviour change and improve adherence is health coaching. In recent years there has been a growing body of evidence showing that health coaching is a beneficial intervention to address weight loss and physical activity in a variety of chronic diseases such as diabetes, myocardial infarction, cancer and chronic Pulmonary disease. Evidence of its use in the low back pain population, however, appears to still be in its infancy and current randomised clinical trials vary substantially in terms of the way and how frequently it is delivered. For this reason, no firm consensus has been reached on the value, acceptability and safety of this intervention for patients with low back pain.
In response to increasing hospital readmissions and burden of low back pain, we developed a health coaching intervention based on promoting healthy lifestyle behaviour (e.g. weight reduction, sleep quality, physical activity promotion, pain coping strategies) for patients with low back pain. The goal was to improve management by coordinating patient access to appropriate conservative care and by empowering the patient to better control their disease and reduce disability, pain and rates of unnecessary surgery.
In partnership with the Physiotherapy Department of Royal North Shore Hospital, we provided a telephone support service to monitor patients with low back pain who are discharged from ED.
Pilot study aims were to test:
- The feasibility of the trial procedures, including: screening and recruitment procedures, baseline assessment and data collection procedures
- Delivery process of the intervention components.
- The feasibility of health coaching intervention/goal setting delivery
The evaluation of the pilot process is important to fine tune the delivery of the service at the primary care level, before evaluating its effectiveness in a future randomised control trial.
Of the participants in this pilot study, 100% considered the support phone service was an acceptable and 80% a useful service with 90% of the participants willing to receive the service again if required in the future. The phone contact frequency and length were also considered to be acceptable in 80% and 100% of participants respectively. There was a positive response from participants with regard to both managing their symptoms better and functional improvements reported in 90%.
The pilot study identified that although the educational information was easy to understand, the content could be improved further in order to increase how helpful participants perceive it to be. The most common area of support reported to be of use was advise on exercise and physiotherapist provision of reassurance, pain education and medications.
The analysis of the Emergency physiotherapists feedback, who identified potential participants found that time taken to and difficulty in identifying relevant patients were the main barriers along with the small number of patients that presented during their usual working hours. They also identified the lack time allocated to provide the service due to lack of funding and failure of patients to answer the phone to scheduled calls as further barriers to the service. Failure of participants to answer scheduled calls occurred twice during the pilot study.
Analysis of the time taken from patient identification to patient enrolment into the study also found that the pilot study processes required streamlining to reduce this time from an average of 7.3 days to 2 days.
Ways to reduce this time frame were identified as:
- Requirement of a site coordinator present in the Emergency department in order to identify, appropriately screen patients and to provide study information prior to their discharge.
- Automatic generation of the baseline (enrolment) survey immediately after the completion of the online consent form to reduce the time taken for the patient to be sent and then access this survey prior to their enrolment.
- Provision of the first assessment phone call over weekends as this was identified as the most common delay between study enrolment occurring on a Friday and the initial phone support call unable to be provided until the following Monday.
The phone support service was widely accepted and positively received by the participants involved. Although the clinical outcomes for the pilot study were not analysed as this was not the aim, previous studies providing health coaching style phone support for patients with low back pain have showed that health outcomes are no worse. The economic evaluation of a health coaching phone service has also shown that it reduces the costs of healthcare for those receiving the service in comparison to those who continued with usual care.
The current evolving pandemic situation involving COVID-19 highlights the utility of providing phone or videoconference consultation to patients that require self-isolation, quarantine or are vulnerable. The accessibility and ease of use of such technology would ensure timely support is still provided to those in need whilst protecting the health of the community at large.
The process evaluation of this pilot study has been used to inform the study designs for 2 further new projects:
- ConnectED: Telecare health coaching for patients with low back pain discharged from Emergency Departments
- Deprescribing opioids in patients with low back pain and hip or hip osteoarthritis
You can read more about this project here: Connect Pilot Study final report
Low Back Pain (LBP) - An analysis on its treatment and effectiveness
| Funded by: | Australian Rheumatology Association-(ARA ) |
| Recipient: | Dr Jenny Setchell |
| Intended Department | School of Health and Rehabilitation Sciences- The University of Queensland |
| Project: | Improving delivery of the biopsychosocial approach: enhancing low back pain healthcare practice. |
This project was designed to ultimately improve the healthcare of a common and burdensome condition – low back pain (LBP). This condition is the leading cause of disability worldwide. It places a huge burden on Australian individuals and the economy, with over $9 billion spent on direct and indirect costs for LBP each year. For many individuals LBP is persistent, recurrent and bothersome, impacting on workforce participation and quality of life. With this project we sought to contribute to addressing knowledge gaps regarding approaches to treatment. Commonly used treatment approaches are known to be ineffective or have minimal positive effects. Research now widely advocates a shift from a biomedical approach to a multimodal biopsychosocial approach. However, there have been difficulties applying this complex approach in practice, with disappointing results of existing attempts to change systems to align with the biopsychosocial approach. This may in part be due to the high possibility that, in addition to traditional psychological and social elements, there are numerous other elements to LBP care that may need to be considered, such as clinician-patient relationships, chronic pain stigma/marginalization, and broader socio-political factors and chronic pain.
We examined if and how these factors are missing or overlooked in clinical LBP care and how these issues might be resolved. Our principally qualitative project used established methods of 1) direct observation of patient-clinician interactions (based on ethnographic principles), 2) iterative analysis sessions with consumers, clinicians and researchers (analysed qualitatively, and evaluated with an established framework – the Realist Evaluation Framework) to develop new strategies. Close collaboration between researchers, clinicians and consumers with LBP is embedded in the project.
Our findings highlighted how non-biological aspects of care such as power dynamics (i.e., in both clinician-patient and clinician-clinician relationships), interprofessional practices, the physical layout of the clinic, and routine daily practices (e.g., the use of computers to gather patients’ information and clinicians’ body language) were usually under-explored at the multidisciplinary pain service. This affected interactions with patients and likely their outcomes. Through our closer collaboration with clinicians and consumers with LBP we were able to develop recommendations to attend to these broader aspects of care. Recommendations included:
- Clinicians adopting an open body language and limiting their use of computers or changing the way they gathered information during consultations with patients;
- Clinicians attending to patients’ physical and emotional comfort throughout the sessions
- An increase in time for the daily multidisciplinary team meeting to address more complex cases and discuss broader aspects of care
- A better attention to interprofessional practices such as addition of discussion about the clinic’s identity and power dynamics between the team members as part of the clinic’s agenda
- Setting up a transition plan for discharging patients from the pain service, with referrals to services and activities at the community level
These elements go beyond the usual use of the biopsychosocial approach to enhance further aspect of care. Through our in-depth exploration of actual practices and collaboration with clinicians and consumers, we were able to develop and support clinicians to implement feasible and practical recommendations to better attend to broader aspects of LBP care. This had direct positive effects on the clinic involved and has had broader impact through the dissemination strategies we have already implemented and will have further impact as we finalise a number of academic publications and other outputs.
The research aims were to:
- to investigate how the psychosocial+ aspects of care do/do not manifest in the clinical management of individuals with chronic LBP at a major public tertiary hospital’s multi-disciplinary pain clinic;
- to develop, implement and evaluate feasible site-specific recommendations at the study site, using an established evaluation framework; and
- to develop and disseminate broad, industry-wide principles to reduce the burden of LBP on individuals, families, communities and the economy – using cross-comparison of implementation outcomes with those from a previously studied private clinic.
Studying these factors is important as it is already having have significant local and distributed impact on Australian and international LBP rehabilitation for three key reasons. The project is: 1) inherently translational: it tested a knowledge translation strategy and this has direct translational effects by enhancing the clinical care in the study site clinic and develops the strategy for wider roll-out across sites (national grants submitted for this). 2) addresses a major health issue: LBP is the leading global musculoskeletal problem, which contributes significantly to personal and community health burden. Enhancing the psychosocial+ aspects of care is likely to reduce the personal, community and economic burden of LBP. 3) contributes to a paradigm shift: this project extends existing research to enhance the delivery of the biopsychosocial model in LBP healthcare, responding to the now considerable transdisciplinary research findings that highlight a need for such a shift but has found it difficult to facilitate.
Although multidisciplinary pain services are considered an optimal setting to pain management, our findings suggest that certain social and broader dimensions of care (psychosocial+) were little attended to in practice. Biomedical and certain psychological dimensions were prioritised. In collaboration with clinicians and people with lived experience with chronic pain we developed and implemented recommendations to address these gaps between desirable and actual multidimensional practices. For example, collaboratively setting up goals with patients, attention to non-verbal communication and usage of computer screen, longer discussions of psychosocial+ aspects of care in team meetings, arrangement of transition plan to the community, and time to develop the service’s team dynamics, were some of the recommendations developed. Recommendations were flexible and took into consideration the service’s specific context in order to enhance the possibility of implementation. The flexible, specific, and collaborative nature of this study is likely to lead to long-term changes to service’s staff and patients and contribute to better attention to social and broader dimensions of care. The project was designed to qualitatively evaluate the changes. During the project there were significant changes to clinic structure, identity, processes and procedures. These multiple changes were reported to enhance patient care and the efficiency of the clinic. The clinicians report that people living with persistent pain are receiving more targeted services and that wait lists have been reduced due to care being more appropriately directed.
The multidisciplinary pain service has already implemented some changes in their clinical and administrative routine, as better explained in the sections above. Clinicians have already implemented changes in their consultation and team dynamic that directly enhance attention to psychosocial+ aspects of patients with musculoskeletal pain including advancing social prescribing. Other administrative changes (e.g., setting up transition/discharge plans) are in the initial stages of implementation, but are likely to benefit people who are referred to the pain service more broadly due to an enhanced efficiency. Our findings will help inform further research in multidisciplinary pain services (and other settings) to go beyond a biopsychosocial approach and consider broader aspects that impact the lives of people with musculoskeletal pain. Our research design provides an example of a productive co-design process which indicates how it is possible to collaborate with clinicians and people with lived experience to develop recommendations that are feasible and targeted to each services’ needs and context. The process might be replicated in a variety of settings when designing, enhancing or redesigning services.
We have agreement with another 2-3 sites to expand the project to other persistent pain clinics and have submitted a grant for funding for a project commencing in 2022. This will also expand the project beyond low back pain to all forms of non-cancer persistent musculoskeletal pain. We have also secured support to conduct a similar methodology in specialised outpatient spinal clinics (OPSCs) which provide non-surgical options to appropriate patients who were referred for spinal surgery. These projects (amongst other potential avenues) will expand our understandings across more contexts and broaden the potential impact of the work.
You can read more about this project here: Scientific Report – J Setchell
Lupus – An Indigenous Australian perspective on diagnosis and treatment
| Funded by: | AFA/ARA Heald Fellowship |
| Recipient: | Dr Fabien Vincent |
| Intended Department | Rheumatology Group, Centre for Inflammatory Diseases- Monash University |
| Project: | Identification of molecular signatures in Indigenous Australians with systemic lupus erythematosus. |
The health disparity between Indigenous and non-Indigenous Australians is a national tragedy. My research program tackles a devastating autoimmune disease called ‘lupus’. Lupus affects about 1 in 1000 people across the population. However, for reasons unknown, this is two to four times more common (and more severe) in Indigenous Australians. My vision is to unravel the reasons for this and use this knowledge to improve the lives of Indigenous Australians with lupus. To do this, we plan to take blood from patients and measure many thousands of genes and proteins. Using complex data analysis methods, known as bioinformatics, we will analyse all these blood markers at once.
This study will establish a national Indigenous lupus registry and biobank (a library for blood and other biological material) and will allow doctors in the near future to find the right drug for the right patient. It will also ensure that Indigenous Australians suffering from lupus will not miss out on breakthrough treatments, or be needlessly exposed to ineffective medicines. Ultimately, this is an important step to closing the health gap between Indigenous and non-Indigenous Australian lupus sufferers.
During my Fellowship, significant progress has been made to set up a national Indigenous lupus registry and biobank, nested within the Australian Lupus Registry & Biobank (ALRB), including logistics and legal aspects in the Northern Territory. We have been successful in obtaining Ethics and Governance approvals to start the recruitment of patients with lupus in key participating sites where most of Indigenous Australians with lupus are expected to be enrolled. We have also obtained more funding for this project from several organisations. Finally, in a pilot study, we have found that the measurement of hundreds of proteins in the blood can help to group patients with lupus into distinct groups. The program is on track for its long-term objectives.
We don’t know why Indigenous Australians suffer more frequently and more severely from lupus compared to non-Indigenous Australians. This may be due to a combination of risk factors, that have not yet been characterised. This knowledge gap needs to be filled to gauge which “biological pathways” are driving illness in Indigenous Australians with lupus, in order to prescribe them the most effective treatments. Importantly, this knowledge will help to make sure ineffective treatments are not used in Indigenous Australians patients suffering from lupus.
We have shown that the measurement of many proteins in the blood of lupus patients can help to group (or cluster) the patients into distinct sub-groups. The grouping of patients was carried on using complex data analysis methods, known as bioinformatics. Importantly, we found that these groups of patients with lupus were different in term of their symptoms and how severe their illness was. These findings confirm the potential for identifying clinically meaningful groups of patients with lupus based on their blood protein measurement.
In order to set up a national registry and biobank of Indigenous Australian lupus patients, a first step involves getting several legal authorisations. We have been successful in obtaining crucial authorisations from Ethics Committees in Northern Territory to allow the recruitment of lupus patients in the hospitals of Darwin and Alice Springs. This is where most Indigenous Australian lupus patients are expected to be enrolled.
This research program also requires additional of funding to enable the collection of data and blood samples of hundreds of individuals across multiple sites, and the measurement of many thousands of genes and proteins in the blood. We have been successful in obtaining funding from several organisations to support this research program totalling seven awards, including from the National Health and Medical Research Council (NHMRC) and from CSL Limited, an Australian leading biotechnology industry, worth approximately $1 million AUD in total.
Finally, we have developed an important collaboration with Dr James Peters, an expert in lupus bioinformatics working in London. This unique expertise will prove invaluable to this project.
My findings will benefit people suffering from musculoskeletal illness in the near future. The outcomes of our pilot study form the foundation for the analysis of similar blood protein measurement in Indigenous and non-Indigenous Australians with lupus.
My research program is establishing the first ever national registry and biobank of Indigenous Australian lupus. This will build the foundation for numerous translational research outcomes, and will result in better understanding of the illness. This project will determine whether Indigenous and non-Indigenous Australians suffering from lupus can be characterised by the presence of singular markers in their blood, where treatments targeting these pathways are either approved or in the pipeline. Biomarker technology will identify which pathway is dominant and thus potentially support providing Indigenous Australians with lupus early access to treatments that target these pathways. This will also help to ensuring ineffective dugs are not used in these patients, furthermore saving money in the healthcare system. This project could swiftly lead to health policy changes affecting the management and treatment of Indigenous Australians with lupus. Importantly, providing these targeted therapies would improve the health and close the gap between Indigenous and non-Indigenous Australian lupus patients.
With the support supported by the AFA/ARA Heald fellowship, I have been awarded funding including an NHMRC Investigator Grant and industry support from CSL to continue this research program for the next five years. The updated timeline for this research program is as follows below:
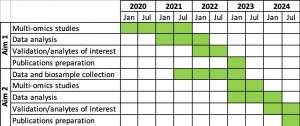
You can read more about this project here: Scientific Summary- Fabien Vincent
The association between cardiovascular disease and gout (gout research fellowship)
| Funded by: | Australian Rheumatology Association- Leanne Stafford Fellowship |
| Recipient: | Dr Ken Cai |
| Intended Department | Bone and Joint Research Group, the University of Auckland and Department of Rheumatology, Auckland District Health Board. |
| Project: | The association between cardiovascular disease and gout (gout research fellowship) |
I completed an overseas research fellowship in Auckland, New Zealand with the support of a grant from Arthritis Australia (Leanne Stafford Award). This grant allowed me to pursue an interest in gout, which is one of the most common forms of arthritis in the community. However, despite having very effective treatments for gout, many people with gout continue to develop permanent disability due to this potentially curable condition. New Zealand is considered the “gout capital of the world” with the highest prevalence of this condition, particularly in people from Māori and Pacific Islander backgrounds. Along with participating in rheumatology clinics, I joined the Bone and Joint Research Group at the University of Auckland working on multiple gout studies under the supervision Prof. Nicola Dalbeth, who is a world-renowned expert in the field. Through completing this fellowship, I wanted to advance my research and clinical skills, with a plan to develop a gout research program back in Sydney, Australia.
During my 12-month fellowship, I spent four days a week at the University of Auckland as a Clinical Research Fellow conducting research in the areas of gout and calcium pyrophosphate deposition disease, another form of crystal arthritis. My remaining time was spent undertaking outpatient clinics at Greenlane Hospital and attending Departmental activities at both Greenlane and Auckland City Hospitals (Auckland District Health Board). Over the course of the year, I authored five original research articles, one review article and presented the results of my research at four international scientific meetings. My research covered a range of topics including the association between gout and cardiovascular disease, the development of a radiographic scoring system for new bone formation in gout and the development of a core domain set for calcium pyrophosphate deposition disease. My research exploring the relationship between cardiovascular disease and gout will form the thesis of my Doctorate, which I am completing through the University of Auckland.
Through my research projects I have developed a collaborative network of colleagues who I continue to work with now that I have returned to Sydney. This includes individual researchers from Europe, USA and New Zealand and research consortiums including OMERACT (Outcome Measures in Rheumatology) and G-CAN (the Gout and Crystal Arthritis Network). We are continuing to expand on projects started during my fellowship as well as commence new projects exploring how to improve gout care and address the increased risk of cardiovascular disease in people with gout. I am also in the process of setting up a dedicated gout clinic for people in Western Sydney, utilising the clinical experience I obtained in New Zealand, particularly around community engagement and improving health literacy in at-risk populations.
I feel very privileged to have had the support of Arthritis Australia to undertake my overseas fellowship. The experience has provided a strong foundation for my research and clinical career, and I will continue to use these skills to improve care for people with gout and other rheumatological conditions.
You can read more about this project here: Scientific Summary – Dr Ken Cai
Arthritis Australia, Paediatric Rheumatology Scholarship
| Funded by: | Australian Rheumatology Association- Arthritis Australia-
Paediatric Rheumatology Scholarship |
| Recipient: | Dr Gráinne Murray |
As part of my current role, supported by the generous scholarship from Arthritis Australia, I have been working on a number of research projects in paediatric rheumatology, aimed at both advancing our knowledge of diseases affecting paediatric patients and at improving patient care.
These projects include
- Patient satisfaction with a switch to a biosimilar medication. Biosimilar medications are usually cheaper than the original brand-name drug although they have slightly different chemical structures, due to the complexity of the large molecules involved, so we have to ensure they work as well as the original. This has been documented in adults, but to a much lesser extent in paediatric patients. My sponsorship by Arthritis Australia has allowed me to observe first-hand the switch by the UK’s National Health Service to treating uveitis (an eye disease that can cause blindness) with a biosimilar, making treatment cheaper. Our project, which is ongoing, is aiming to confirm that this drug works just as well as the original medication, and also to get patients’ feedback on this switch. We are specifically asking patients and their parents about any side effects, to make sure that they are not more of a problem in the case of the biosimilar drug.
- Working with the Global Musculoskeletal Taskforce on a submission to the World Health Organisation (WHO): Many children with arthritis and uveitis in the developing world have little access to treatments considered standard in Australia. This leaves them at increased risk of pain, deformity, growth issues, and blindness. As part of an international collaboration, I have helped with an application to get tocilizumab, a potent immunosuppressant used in the treatment of systemic Juvenile Idiopathic Arthritis (JIA) added to the WHO’s Essential Medicines List for Children
- Review of forthcoming treatments of JIA: my paper, recently accepted for publication by the Lancet Rheumatology journal, summarises worldwide research into the most important recent advances in care, and the likely advances in the next few years.
- Chronic Non-Infectious Osteomyelitis of the Mandible: this is a rare and painful condition where the jaw bones become inflamed. Due to its rarity it can be missed. I have recently had an article accepted to Lancet Rheumatology showing how to better recognize the condition to raise awareness among other doctors, leading to earlier diagnosis and better outcomes for patients.
- I have also helped recruit and assess patients for the following drug studies: ADJUST (Adalimumab in JIA Associated Uveitis Stopping Trial) and the trials for Baricitinib (JAK inhibitor) in uveitis and polyarticular JIA, a form of JIA which affects multiple joints.
As part of this scholarship, I wanted to improve our knowledge of the treatment of uveitis. I chose to use the scholarship working at Bristol Royal Hospital for Children for its expertise in this disease. Attending joint uveitis clinics with their consultant rheumatologist and ophthalmologist, I have learnt how to optimise joined-up care for these patients. In discussion with my supervisor, I chose to research how well biosimilars work and how the patients find them. I had suspected that Australian funders such as the Pharmaceutical Benefits Scheme would soon require patients to switch to the cheaper biosimilar drugs, and this is now happening, so my witnessing the UK experience will really help doctors, patients, and their parents as the changeover rolls out in Australia.
In working with the WHO taskforce, I aimed to improve the standards of care for children in developing countries who have JIA. Several medications used for children living in Australia, the UK, and other developed countries are expensive and so have limited availability worldwide contributing to childhood disability and pain. I have therefore searched the literature and done a cost analysis, together with members of a global taskforce, and submitted this to the WHO for consideration. If a medicine can be added to the WHO’s Model List of Essential Medicines for Children, it makes it easier for developing countries to prioritise cost-effective treatments. Increasing awareness of how many children suffer without these medications is also important to ensure that they will be added to the Essentials Medicines List. This document is currently under review with WHO with a response expected in mid 2021.
Although some of the research has been delayed due to the COVID-19 pandemic, to date it appears that the cheaper medication is just as effective at controlling the patient’s disease, as I had expected. However, several patients have reported that the new medication (which is administered by an injection once per fortnight, as diabetics do for insulin), is more painful to administer than the medication they were on before and so they want to switch back to the original medication. This is a big concern for parents who are administering injections to their children, often for many years. As this idea of biosimilar switching is very new to paediatrics, there is little information published about patients’ views on it, so I hope that completing this project in the coming months will improve our knowledge and awareness of the potential difficulties.
In my audit of Chronic Non-Infectious Osteomyelitis of the jaw, I described several novel factors and considerations in the diagnosis and management of this condition. For example, the disease is more likely to be isolated to a single bone, the mandible (jaw), and is more likely to be resistant to first-line treatments.
Although some of my projects are not fully completed or published yet, there are some early benefits for patients with musculoskeletal diseases. I presented my audit of chronic non-infectious osteomyelitis of the jaw to our local team meeting, which helped to raise awareness and discussion among team members of this unusual condition. My editorial on scoring systems for patients with systemic JIA has also been published in Rheumatology, Oxford Press and will hopefully be widely read.
As I am now analysing the data for the uveitis patients about the switch to biosimilars, I cannot comment in detail yet, but I intend to publish my recommendations to both the medical community and to patient organisations, so that both groups are ready for this upcoming change.
The WHO taskforce project, has the potential to have significant impacts on sufferers of musculoskeletal disease worldwide. In developing countries this could significantly change a child’s life, particularly if they can avoid significant disability such as limb deformities and chronic pain. It will enable them to lead a normal life, with the ability to pursue their chosen career and integrate normally in society. It will also have significant effects for the wider family and community in not having a disabled child to care for.
My review of current treatments available aims to support doctors worldwide in keeping up with advancing knowledge in JIA. With so many potential new medications it is important that staff know all the options for patients and avoid delay in giving the best treatment.
I have not yet completed my project on biosimilar switching in uveitis, and therefore I will aim to complete and publish this in the coming months. I intend to remain involved with clinical research through my links with the Bristol team, and to work collaboratively with them from Australia to improve knowledge and outcomes for patients in both countries.
I plan to continue my involvement with the ADJUST study in particular, which continues in Bristol and will be running at RCH Melbourne while I am in post there from February 2021.
Rheumatic diseases- A patient reported outcome (PROM)
| Funded by: | Australian Rheumatology Association & Arthritis Australia |
| Recipient: | Prof Catherine Hill |
| Intended Department | University of Adelaide |
| Project: | Development of a patient reported outcome measure (prom) for glucocorticoid impact in rheumatic diseases |
Glucocorticoids (GCs) are widely used in the rheumatic diseases, including rheumatoid arthritis, vasculitis, lupus, and giant cell arteritis.
They are an effective therapy which can be life-saving but have significant adverse effects. We are developing a patient reported outcome measure (PROM), or standardised questionnaire, to measure the impact of glucocorticoid use on patients’ symptoms and health-related quality of life. This will be used in clinical care to target treatment or clinical trials of steroid-sparing agents.
Qualitative patient interviews were conducted in Australia (n=10), United Kingdom (n=35)
and USA (n=10) by experienced qualitative researchers. Patients with a range of demographics, rheumatic diseases and levels of GC exposure across three continents were recruited in Adelaide for the Australian interviews. Following transcription of these interviews in Australia, these were collated with the interview transcripts of those from UK and USA.
Thematic analysis of these interview as well as data from previous interviews undertaken as part of the Glucocorticoid Impact Working Group of OMERACT (Outcome Measures in Rheumatology) were used to draft the first iteration of the GC-PROM. This work has been supported by the OMERACT GC Working Group which has involved a patient research partner.
We held a virtual international workshop in October 2020 which endorsed the core domain set for measuring of outcomes in GC which has recently been published (reference below).
We are currently undertaking cognitive interviews of the draft of the GC-PROM which will determine patient acceptability and understanding.
There have been some delays to the project mainly due to the COVID-19 pandemic in UK and USA.
We are now seeking funding for a larger validation study.
We sincerely thank Australian Rheumatology Association for the funding; and Arthritis Australia for support, which has allowed the research to be carried forward. We would also like to thank the participants of our study who gave their time for our research.
Reference: Tieu J, Cheah JT, Black RJ, Christensen R, Ghosh N, Richards P, Robson J, Shea B, Simon LS, Singhi JA, Tugwell P, Boers M, Garibay MAA, Campochiaro C, Decary S, de Witt M, Fernandez AP, Keen HI, King L, Hinojosa-Azaola A, Hofstetter C, Gaydukova I, George MD, Gupta L, Lyne S, Makol A, Mukhtyar C, Oo WM, Petri M, Pisaniello HL, Sattui SE, Russell O, Teixeira V, Toupin-April K, Uhunmwangho C, Whitstock M, Yip K, Mackie SL, Goodman SM, Hill CL. Improving benefit-harmassessment of glucocorticoid therapy incorporating the patient perspective: The OMERACT glucocorticoid core domain set. Semin Arthritis Rheum. 2021 Jun 25:S0049-0172(21)00122-0. doi: 10.1016/j.semarthrit.2021.06.010. Epub ahead of print.
Sign up to Arthritis Insights
Regular updates, news and research findings delivered to your inbox: