Reports
The future burden of arthritis in Australia: Projections to the year 2040
With 1 in 6 expected to suffer from arthritis, these individuals face significant health challenges in their prime years. Over 5.3 million Australians are projected to grapple with arthritis by 2040, marking a 31% increase from today’s figures. This surge in arthritis cases demands urgent attention, with serious economic and workforce implications looming.
Women, in particular, will bear the brunt, facing nearly 80% higher rates of osteoarthritis than men. Arthritis Australia CEO Jonathan Smithers emphasises the need for proactive measures to address this escalating health crisis.
To tackle these challenges head-on, Arthritis Australia proposes three key actions:
1. Allocate resources and funding for affordable access to care and research.
2. Raise awareness and challenge misconceptions about arthritis, promoting early intervention.
3. Address barriers to daily activities and inclusion in workplaces and social settings.
These projections highlight the critical importance of taking action now to support those affected by arthritis and safeguard our future.
Arthritis Australia Consumer Research Activity Report (2020)
People with arthritis are at the centre of Arthritis Australia’s mission and activities, and consumer-based research underpins our policy development and advocacy.
In 2018-19, the major focus of our consumer research related to identifying consumer issues and action priorities for the development of the National Strategic Action Plan for Arthritis. In addition, consumer research was undertaken to inform Arthritis Australia’s responses to government consultations and inquiries.
National Strategic Action Plan for Arthritis (2019)
The National Strategic Action Plan for Arthritis provides an evidence-informed blueprint to guide national efforts to improve health-related quality of life for people living with arthritis. Implementing the Plan will help to reduce the cost and prevalence of the arthritis and reduce its impact on individuals, their carers and the community.
Arthritis is one of the most common, costly and disabling of all chronic conditions. Nearly four million Australians of all ages, including children and young people, live with arthritis. Yet the personal, social and economic impact of arthritis is poorly recognised and often wrongly trivialised.
We can do much to prevent and better manage arthritis to reduce the severity of the condition and its impact on individuals, carers and families, health and welfare systems, and the economy.
The Action Plan identifies three key priority areas and a range of actions to achieve the overall vision of freedom from the burden of arthritis.
Stakeholders across all sectors of the health system will need to work together to implement the Action Plan.
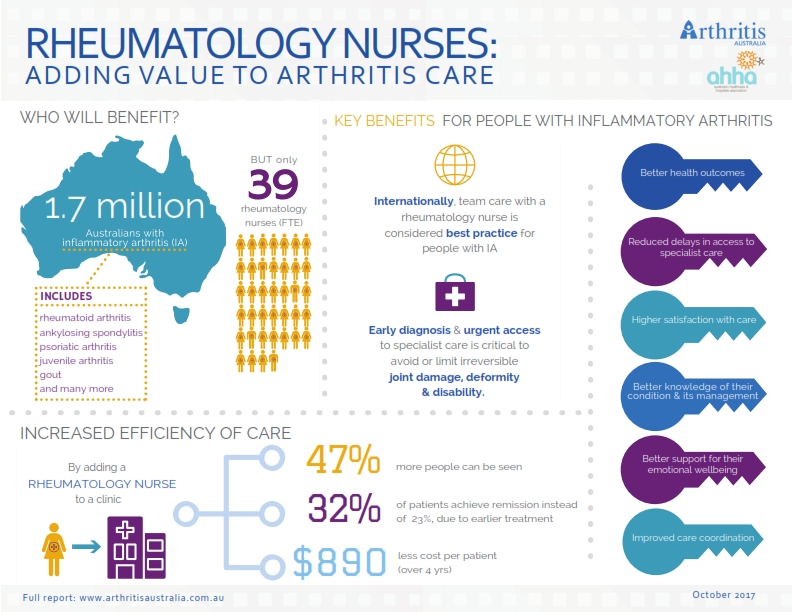
Rheumatology Nurses (2017)
Rheumatology nurses could be the answer to improving care for hundreds of thousands of Australians with inflammatory arthritis.
Around 1.7 million Australians suffer with chronic, inflammatory forms of arthritis, yet there is a severe shortage of the specialist nurses who are trained to help care for these patients.
The report Rheumatology nurses: Adding value to arthritis care looks at the evidence supporting the benefits of rheumatology nursing and assesses access to rheumatology nursing care in Australia. The report commissioned by Arthritis Australia, found that there was just one full-time rheumatology nurse for every 45,000 people living with painful and disabling conditions such as rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis, gout and juvenile arthritis.
“An increase in rheumatology nurses would mean quicker diagnoses, better psychosocial support for patients, improved quality of care, better patient outcomes and reduced health system costs,” Ms Cahill said. “Importantly, this research confirms that people who see a rheumatology nurse as part of their care are much more satisfied with all aspects of their care than those who do not.”
“Adding rheumatology nursing to the traditional care model which uses only a rheumatologist would mean quicker access to specialist care and an earlier start to treatment. Our report shows this would in turn mean an increase in the number of patients going into remission and a decrease in the average cost of care per patient,” said Ms Cahill.
“For these reasons, we call on the Federal, State and Territory governments to provide dedicated funding to train and employ more rheumatology nurses,” finished Ms Cahill.
Literature review: Rheumatology nurses
Counting the cost (2016)
A major report shows the growing multi-billion dollar costs of arthritis to the economy, individuals and to the healthcare system and how relatively small investments could yield savings of more than $170 million a year.
Key findings of the report include:
- There are 3.9 million Australians with arthritis and this will grow to 5.4 million by 2030.
- Arthritis currently costs the health system $5.5 billion and this will grow to $7.6 billion by 2030 unless more is done to prevent and better manage the condition.
- Arthritis is a major cause of disability and early retirement due to ill-health. This costs the government $1.1 billion in extra welfare payments and lost taxation revenue and costs the economy $7.2 billion in lost GDP alone.
- Providing better care for people with arthritis can save the health system over $170 million a year by reducing demand for joint replacements.
Arthritis and Disability (2014)
Arthritis is a leading cause of disability in Australia
This study was undertaken to better understand the lived experience of people with arthritis. A total of 819 people with arthritis volunteered to participate in this study through a consumer focus group (13 people), individual one-on-one interviews (28) and an online survey (778).
The impairment associated with arthritis varies significantly, depending on the type and severity of the condition, the presence of other health conditions, and the time since diagnosis. The level of disability experienced by people with arthritis also depends on a variety of factors, including access to informal and formal support, flexibility in the workplace, and the availability of measures for social protection.
People with arthritis-related disability become socially excluded across one or more and sometimes all life domains – study, work, family and social participation. In particular, people’s capacity to work is adversely affected by arthritis, with implications for their ability to meet the often high costs of managing their condition and to maintain an adequate standard of living.
Key Findings:
- Nearly all participants (95 per cent) reported that their arthritis limited their ability to engage in daily activities, with 37 per cent reporting that they were always limited.
- People with arthritis reported significantly lower wellbeing compared with the general Australian population with the greatest adverse impact occurring in the domains of health, employment and finances.
- Carers of people with arthritis also reported significantly lower wellbeing than that of the general population (66.0 compared to 77.6)
- 67 per cent of all participants reported that arthritis had affected their ability to work or study, now or in the past; 23 per cent reported that they were permanently unable to work or study because of their condition; 68 per cent were restricted in the type of work or study they could do; and 65 per cent were restricted in their hours of work or study.
- Participants reported that the financial consequences of their arthritis were detrimental due both to the high costs associated with living with the condition and the loss of income due to reduced capacity to work. Costs included: ongoing medical care; the high and continual cost of medications; aids and equipment; home help and maintenance services; personal care; and transport.
Time to Move (2014)
The Time to Move: Arthritis strategy provides a road map for improving care across Australia for people with arthritis, addressing the spectrum of intervention from prevention to advanced disease. The strategy was developed with the input of a multidisciplinary steering committee comprising experts from rheumatology, general practice, pharmacy, patient advocacy, allied health and key services. Stakeholder consultations were also held across Australia in the course of developing the strategy.
Key points
- Arthritis is one of the most common, disabling and costly chronic diseases in Australia. It affects more than three million people of all ages with more than half of those affected being of working age.
- Arthritis costs the health and welfare systems more than $5.6 billion annually.
- The loss to the Australian workforce is highly significant. More than 80,000 people aged 45 to 64 years can’t work because of their arthritis, at an estimated loss to GDP of $9.4 billion a year and a cost of about $1.3 billion annually for the Disability Support Pension.
- As the population ages, the number of people with arthritis is expected to reach seven million by 2050.
- Yet the management of arthritis in Australia falls well short of best practice. Two thirds of people with arthritis say they are faring badly, over half of people with the most common form of arthritis (osteoarthritis) don’t receive care in accordance with current guidelines and most GPs are dissatisfied with the care they are able to provide.
- Many people with arthritis face limited services, inequity of access, delays in diagnosis and treatment, fragmented care that is rarely multidisciplinary, inadequate support for self-management, a lack of psychosocial support and a heavy financial burden.
- A substantial proportion of the cost and burden of arthritis could be reduced by adopting prevention strategies and improving the care and support we provide for people with arthritis.
- The Time to Move strategy provides a road map for improving care across Australia for people with arthritis, addressing the spectrum of intervention from prevention to advanced disease and identifies key recommendations to support implementation.
The key components of the strategy are:
- awareness raising campaigns and strategies
- health promotion and primary prevention strategies
- enhanced education and self-management support for people with arthritis
- community based multidisciplinary arthritis clinics and teams
- workforce capacity building, including enhancing support for primary care to provide effective management of people with arthritis
- research
Researching our Research (2014)
The importance of high quality, well-targeted research to deliver solutions for debilitating diseases such as arthritis can’t be overstated. The development and implementation of new and improved therapies, diagnostic techniques and clinical policies can take decades to achieve through dedicated research funding and career support for talented researchers. As a proud funder of arthritis research in this country for 30 years, Arthritis Australia is committed in its contribution to this immense research effort.
Key points
- Australian researchers are doing all that they should to drive medical research, publishing their research in high quality journals, collaborating nationally and internationally and leveraging further funding.
-
Most of the early career researchers we have supported over this period are still active contributors to the field, with over a quarter achieving promotion.
- Other standout achievements include the rate at which Arthritis Australia researchers go on to win further funding, with nearly a third awarded highly esteemed NHMRC grants – an indicator of the quality of the foundation Arthritis Australia research that led to these awards.
- Nearly a quarter of the researchers holding Arthritis Australia grants over this period have received a prize or other measure of professional esteem.
The Voice of GPs on Arthritis (2012)
A 2011 Arthritis Australia survey of people living with arthritis showed that those who were not faring well with their arthritis considered it was due to their perceived standards of care and access to care and information, rather than the severity of their arthritis, how long they’d had it, their age, their income, private health insurance cover nor other illnesses.
Since these findings implied criticism of medical care and in particular of General Practitioners (GPs), a survey of GPs’ views was undertaken in order to ‘hear the other side’ and formulate a collaborative strategy for action. The research for this report was focused on treatment of Australians with osteoarthritis and rheumatoid arthritis. The research was conducted through a combination of qualitative group discussions, individual in-depth interviews and a quantitative survey across a nationally representative sample of GPs.
Key points
- The findings of the Voice of Arthritis consumer survey of 2011 are largely explained by these results.
- The burden of OA in the community is reflected in the load GPs carry.
- There’s a degree of ‘heart sink’ among GPs about OA.
- They know OA is important and want to do more for their patients but feel somewhat isolated and helpless and, consequently, a significant proportion develop therapeutic defeatism.
- A proportion of GPs identified people with OA as having complex issues and perceive them often to be ‘difficult’ patients with unrealistic expectations.
- There is poor awareness among GPs of the resources available to them, including non-drug treatment options that they might be routinely using.
- GPs are underutilising their practice nurses in the care of people with OA.
- GPs want more skills and tools to assess and manage pain and disability better
The Voice of Arthritis (2011)
Voice of Arthritis 2011 was a community based survey which recruited a representative sample of over 1000 people with arthritis across Australia. The purpose was to find out how arthritis affected people at home and at work and what factors were associated with good or poor outcomes.
Key points
- About a third of people were coping quite well with their arthritis, 52% were doing fairly badly and 16% were doing badly.
- The two groups which were doing worse represented over two thirds (68%) of respondents. People in these groups experienced significantly more pain, disability leading to a reduction in their work capacity, increased financial strain and social isolation.
- A large proportion of people with arthritis (79%) also reported another condition such as heart disease, high blood pressure, diabetes or depression and in over half the cases, these conditions followed the diagnosis of arthritis.
- The worse someone was faring with their arthritis was associated with their perceived standard of care, the information made available to them, and access to care – not with the severity of their arthritis, how long they have had it, their age, their income, private health insurance cover nor other illnesses.
Painful Realities (2007)
This report, prepared for Arthritis Australia, assesses the economic costs to Australia of one of the country’s most prevalent diseases, arthritis. There are more than 100 known types of arthritis, the most common being osteoarthritis (OA), rheumatoid arthritis (RA), systemic lupus erythematosus (SLE or lupus), gout and spondyloarthropathies.
Key points
- Nearly one in five Australians has arthritis; indeed more Australians have arthritis than any other national health priority condition.
- In 2007, there are an estimated 3.85 million Australians with arthritis, including 2.4 million in the working age population (15-64 years).
- It is estimated that 78% of people with arthritis reside in New South Wales, Victoria and Queensland, indicative of the concentration of Australia’s population on the eastern sea board.
- By 2050, it is projected there will be 7 million Australians with arthritis – 23.9% of the projected population of 29.4 million.
- In 2007, the total cost of arthritis to the Australian economy is estimated to be $23.9 billion, an increase of more than $4 billion on the cost calculated by Access Economics in 2004.
Sign up to Arthritis Insights
Regular updates, news and research findings delivered to your inbox: