Steroids (children)
What are steroids?
Steroids are hormones that occur naturally in the body. They are used as medications to treat certain childhood rheumatic conditions (diseases which may affect joints, muscles, bones, skin or eyes). This can include juvenile arthritis (JIA), lupus (also known as SLE), uveitis, dermatomyositis and scleroderma. Steroids work by affecting the immune system and reducing inflammation. They have been safely used for over 50 years. They are the most common medications used by rheumatologists. Steroids are also used for other types of diseases, such as asthma and eczema.
How will it help?
Steroids work quickly to reduce inflammation. They suppress the immune system which is overactive in autoimmune conditions like JIA, lupus, uveitis and dermatomyositis. How are steroids given? Prednisolone (the most commonly used steroid) can be swallowed as a tablet or liquid. It is usually taken once or twice a day. It is usually taken in the mornings with food. Other steroids can be given as creams, eye drops, or injections into the veins or joints. Your child’s particular condition will help decide on the dosage method and your doctor will talk to you about this.
What is the dose?
This depends on the size and weight of your child. It also depends on how bad the disease is. A higher dose will be used initially. Your doctor will try to lower the steroid dose as the disease improves. Sometimes the dose may be increased if the disease gets worse or the body is under stress from infection.
How long will it be used for?
This will depend on your child’s condition and how they respond. Sometimes steroids are used for just a few days and sometimes they are required for many months.
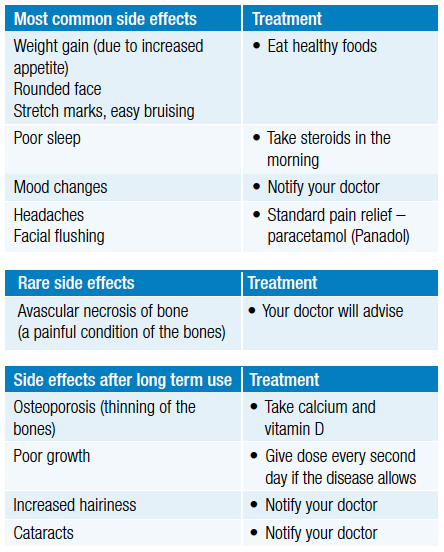
Are there any side effects?
Low dose prednisolone taken for a few weeks does not usually cause any side effects. If steroids are needed in high dose or for a long time, certain side effects are more likely. Most of these disappear once the steroid is stopped or reduced.
Things you need to know when taking this medicine
Your child will be carefully monitored while on steroids. This includes checking their growth, weight, blood sugar level, sodium levels, blood pressure, eye examinations and bone density (in long term steroid use). If steroids have been taken for more than a few weeks, it is dangerous if they are stopped suddenly. Instead, steroids need to be reduced slowly over time.
What to do if your child is sick
Steroids should still be given if your child is unwell. If they have vomited after taking their dose, please talk to your doctor.
Interactions
Steroids are generally safe to take with other medications. There are some natural and herbal preparations that contain steroids, so check with your doctor before you use these medications.
Immunisations
Most immunisations are safe to give (flu vaccine, cervical cancer vaccine, killed polio vaccine (IPV) etc) when taking steroids. Live virus vaccines (such as mumps, measles, rubella (MMR), polio (OPV)) varicella (chicken pox) and some travel vaccines should not be used if you are on high dose steroids. Check with your doctor or nurse.
Infections
There is an increased risk of some infections if you are on high dose steroids.
Myths and misconceptions
The steroids used for inflammation are not the same as those abused by some athletes. You may hear a lot of different information about steroids from friends, pharmacists or people you know. If you are worried about anything, please talk to your doctor or nurse for more information. If your child is taking steroids they should see their paediatric rheumatologist regularly to make sure their treatment is working and to minimise any possible side effects.
This medicine should be kept in a safe place, as accidental overdose can be serious.
Important things to remember
- You must see your rheumatologist regularly to make sure the treatment is working and check for possible side effects.
- You should have regular blood tests as suggested by your rheumatologist.
- If you are worried about any side effects, you should contact your rheumatologist as soon as possible.
- If you stop steroids for any reason, you must contact your rheumatologist.
For further information see Steroids printable Information sheet_Paediatric
This Information Sheet has been prepared using materials obtained from various sources which have been reviewed by the Australian Rheumatology Association (ARA). It contains general information only and does not contain a complete or definitive statement of all possible uses, actions, precautions, side effects or interactions of the medicines referenced. This information is not intended as medical advice for individual conditions nor for making an individual assessment of the risks and benefits of taking a particular medicine. Decisions regarding the assessment and treatment of patients are the sole responsibility of the treating medical professional, exercising their own clinical judgment and taking into account all of the circumstances and the medical history of the individual patient. ARA has used all reasonable endeavours to ensure the information on which this Information Sheet is based is accurate and up to date. However, the ARA accepts no responsibility or liability for the accuracy, currency, reliability and/or completeness of the information contained in this Information Sheet. To the maximum extent permitted by law, the ARA expressly disclaims any liability for any injury, loss, harm or damage arising from or in connection with use of and reliance on the information contained in this Information Sheet. This information sheet is copyright and may be reproduced in its entirety but may not be altered without prior written permission from the ARA. Page updated April 2024Discover more...
-
Advocacy & policy
Arthritis Australia advocates to government, business, industry and community leaders to improve care, management, support and quality of life for people with arthritis..
-
10 steps for living well with arthritis
Here is our 10 steps checklist to help you live with arthritis.
-
Programs & Research
Arthritis Australia funds research and advocates to improve care, management, support and quality-of-life for people with arthritis.
Sign up to Arthritis Insights
Regular updates, news and research findings delivered to your inbox: